Multiple sclerosis
Direct application of biopharmaceuticals through the nose into the brain
There is currently no cure for multiple sclerosis, the most common neurological autoimmune disease in humans. Biopharmaceuticals that can delay the course of the disease or diminish its effects are often prevented from being fully effective by the blood-brain barrier. A European consortium led by the Fraunhofer IGB, Stuttgart is developing a new technology that can transport an innovative active ingredient directly to the central nervous system via the olfactory mucosa in the nasal cavity, bypassing the blood-brain barrier. This will improve the treatment of multiple sclerosis.
Multiple sclerosis (MS) is by far the most common autoimmune disease of the central nervous system (CNS) in the world, affecting around 700,000 people in Europe and an estimated 2.3 million worldwide. The first signs of MS often appear in young adulthood, from the age of 20 or even earlier. MS is second only to road accidents as the most common cause of disability in young adults. The disease often begins with optic nerve inflammation, which causes retinal damage to the eye, and leads over years or decades to an increase in neurological dysfunctions such as numbness, nerve pain and paralysis. The economic cost of MS is enormous: according to studies by the European Multiple Sclerosis Platform (EMSP), the umbrella organisation of the 40 European MS specialist societies in 35 countries, 80 percent of MS sufferers are no longer able to work within 15 years of initial diagnosis - often in the most productive phase of their lives.
Variable disease pattern and no cure for MS
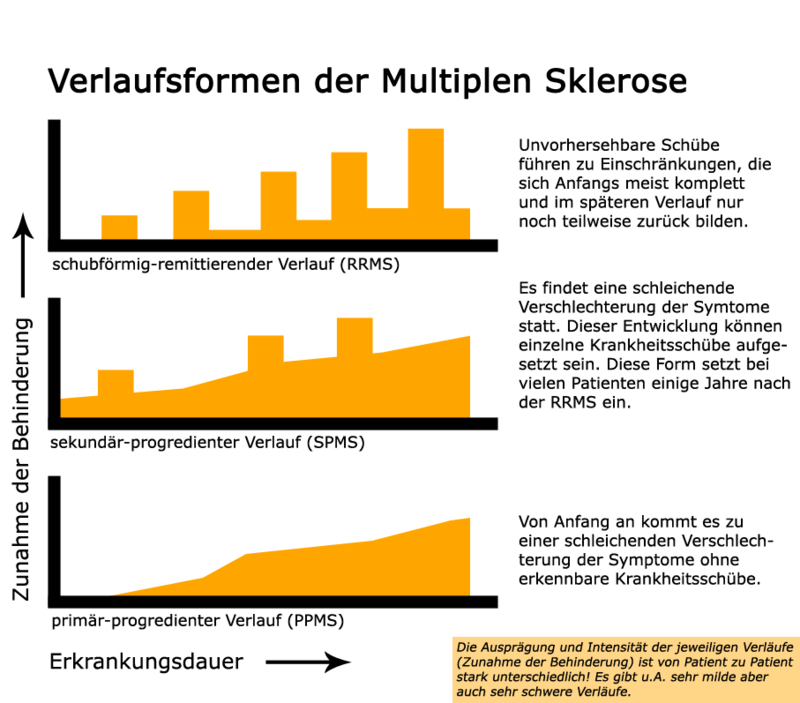 Multiple sclerosis can take several forms. Source: Vhancer https://de.wikipedia.org/wiki/Multiple_Sklerose# /media/Datei:Verlaufsformen-MS.png (CC0)
Multiple sclerosis can take several forms. Source: Vhancer https://de.wikipedia.org/wiki/Multiple_Sklerose# /media/Datei:Verlaufsformen-MS.png (CC0)MS causes damage to the myelin sheaths that surround the nerve processes in the CNS. This disrupts the transmission of the nerve signals, and the nerve cell ends up dying. Inflammatory lesions develop in many places along the nerve pathways, and can be easily detected by magnetic resonance imaging. These inflammatory lesions can harden over time - hence the name "multiple sclerosis". It is known that the body's own immune cells play a part in the development of MS, but the actual cause of the disease is still a puzzle. So far there is no cure. The course and symptoms of the disease can vary considerably: disabilities can develop relatively quickly or over decades, and occur in episodes (which can partially or fully regress) or progressively over time (see Figure).
There are different approaches to MS: medication can alleviate the symptoms, and the course of the disease can be delayed or even frozen, sometimes for a considerable period of time. Depending on the type and form of the disease, anti-inflammatory glucocorticoids, immunosuppressive or immunomodulating biopharmaceuticals such as beta-interferons and monoclonal antibodies are used. It is vital that sufficient concentrations of the active pharmaceutical ingredient (API) reach their destination for the treatment to be effective.
The blood-brain barrier and how it can be bypassed
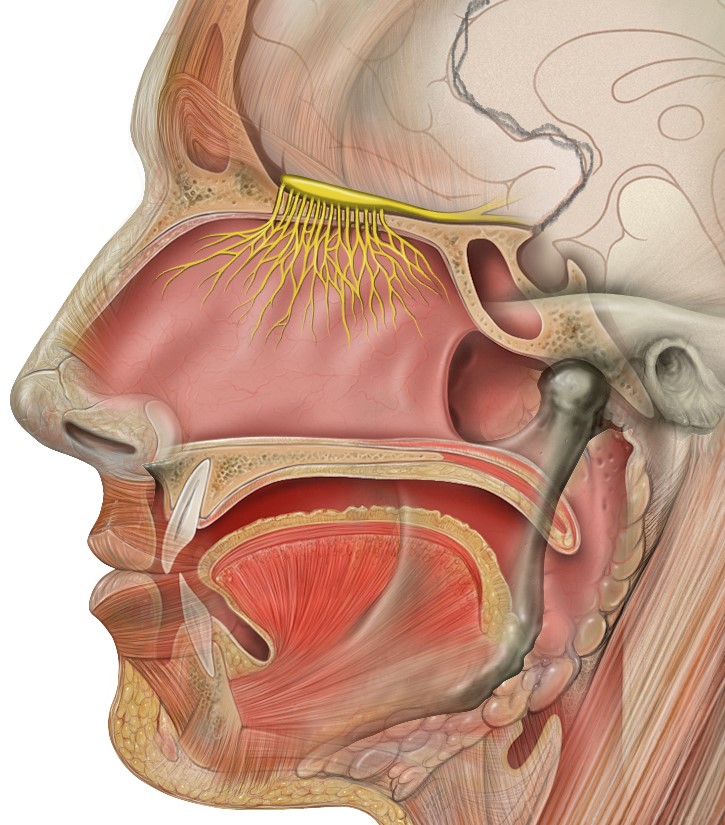 Anatomy of the human head. The olfactory nerve is shown in yellow, as are the branches that start from the olfactory mucosa and lead through channels of the ethmoid bone to the olfactory bulb of the cerebrum. The ethmoid is the part of the skull bone that separates the nasal cavity from the brain. Source: Wikimedia Commons. Patrick J. Lynch, Creative Commons Attribution 2.5 License 2006. https://de.wikipedia.org/wiki/Datei: Head_olfactory_nerve.jpg
Anatomy of the human head. The olfactory nerve is shown in yellow, as are the branches that start from the olfactory mucosa and lead through channels of the ethmoid bone to the olfactory bulb of the cerebrum. The ethmoid is the part of the skull bone that separates the nasal cavity from the brain. Source: Wikimedia Commons. Patrick J. Lynch, Creative Commons Attribution 2.5 License 2006. https://de.wikipedia.org/wiki/Datei: Head_olfactory_nerve.jpgIn the case of MS and other neurodegenerative diseases, the effectiveness of the, often very expensive, biopharmaceutical drugs is limited by the fact that the blood-brain barrier makes transporting the API via the bloodstream or the digestive tract, in the case of oral intake, to the destination (i.e. the damaged areas of the CNS) difficult or even impossible. The blood-brain barrier consists of a layer of endothelial cells around the blood capillaries. The cells are particularly tightly connected to one another, making the layer practically impermeable to many substances.
However, there are gaps in the blood-brain barrier where the nerves emanating from the sensory organs enter the brain. It has been shown in the animal model that therapeutic macromolecules such as neuropeptides, insulin and other hormones, which cannot normally penetrate the blood-brain barrier, reach the CNS quickly via the olfactory nerve in the nose. The transport of macromolecular therapeutic agents into the brain after “intranasal” administration has also been demonstrated for humans. The active ingredients follow the fibre bundles of the olfactory nerve, which lead from the sensory cells of the olfactory epithelium (the olfactory mucosa) in the nasal cavity through fine channels of the ethmoid bone, a bone that separates the nasal cavity from the brain, to the olfactory bulb in the cerebrum (see Figure).
The N2B-patch project in the EU's Horizon 2020 programme
A multidisciplinary consortium led by the Fraunhofer Institute for Interfacial Engineering and Biotechnology IGB in Stuttgart, consisting of eleven partners from eight European countries (Germany, Czech Republic, Greece, Italy, Great Britain, France, Belgium and Switzerland) is developing a technology that enables the intranasal application of APIs for the regenerative treatment of MS. We previously reported on the launch of the programme in 2017 (“N2B-patch: circumventing the blood-brain barrier”). N2B-patch (nose-to-brain delivery of an active pharmaceutical ingredient via the olfactory region) is receiving funds of over 5.3 million euros for a period of four years from the EU’s Horizon 2020 programme. In addition to the active ingredient - an innovative biopharmaceutical as an API for the treatment of MS - the N2B-patch project will deliver three concrete outputs (see Figure):
• an ensemble consisting of API and biomaterial-based drug particles;
• the "patch", a galenic hydrogel formulation as a minimally invasive carrier for the active ingredient;
• a suitable applicator for inserting the gel patch into the nose.
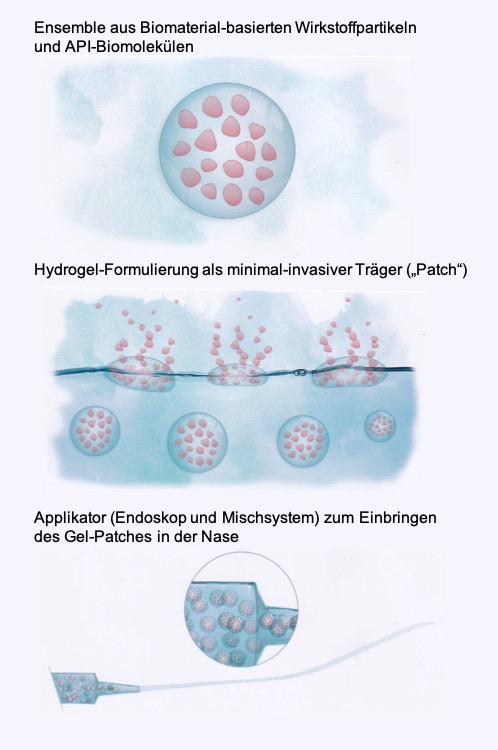 Three main outcomes of the N2B-Patch project in the EU's Horizon 2020 programme. © N2B-Patch (Fraunhofer IGB, C. Gruber-Traub) 2020
Three main outcomes of the N2B-Patch project in the EU's Horizon 2020 programme. © N2B-Patch (Fraunhofer IGB, C. Gruber-Traub) 2020“The scientists at the Fraunhofer IGB are concentrating on formulating the particles that contain the active ingredient and introducing the particles into the gel,” explained Dr. Carmen Gruber-Traub, the coordinator of the N2B-patch project and head of the working group at the Stuttgart IGB. The galenic formulation protects the sensitive biomolecules that make up the active ingredient and ensures that their biological activity is retained. The patch, just a few millimetres in size, a kind of gel plaster, has to be applied to the site of action - the olfactory mucosa - by a doctor with a specially developed device. The olfactory mucosa is located in the rear of the nasal cavity and is difficult to access. The applicator consists of a commercially available endoscope and a special mixing system that stops the gel solidifying before it has been placed in the intended location. The active substance is released from the patch to the olfactory mucosa over a prolonged period and transported to the brain via the channels of the olfactory nerve fibres in the ethmoid bone. The gel dissolves on its own. If long-term therapy is required, a new patch can simply be inserted through the nose.
The idea is to provide proof of concept and carry out the preclinical validation of this innovative approach for more effective treatment of multiple sclerosis by the time the current project ends. Further development, from clinical validation to approval and the marketable product, can then be undertaken in cooperation with the pharmaceutical industry. Gruber-Traub emphasises that the concept of applying drugs via the nose to the brain, which was developed in the N2B-patch project, also has the potential to be used with other active ingredients and correspondingly adapted formulations for treating neurodegenerative diseases such as Parkinson's and Alzheimer's. According to Gruber-Traub, coordinating a consortium within the framework of an EU project and transnational cooperation with partners from different regions also offers a unique opportunity to advance a research topic, build a new network and meet new challenges.