DiHeSys takes steps towards application
Digital Health Systems GmbH (DiHeSys) has completed its founding phase and entered a new stage of development. This is reflected in the arrival of a new managing director, a strategic cooperation and its first pilot projects.

Prof. Dr. Christian Franken joined DiHeSys as managing director on June 1st 2020. As co-managing director alongside company founder Dr. Markus Dachtler, Franken is responsible for marketing, sales, business development and communication. "I’d like to actively create another big business," he says. He wants to help build the small company, increase resources and sales and develop sensible business models for market integration.
Franken’s previous role was chief pharmacist at DocMorris, Europe's largest online pharmacy, before he left the company in late April 2020. In his 13 years at DocMorris, he explored the feasibility of pharmaceutical digitalisation. He believes that digitalised production of pharmaceuticals - since the first pharmaceutical was printed and approved in 2015 - is "extremely relevant for the future", bringing together patient focus and digitalisation.
Strategic alliance with global player Höfliger
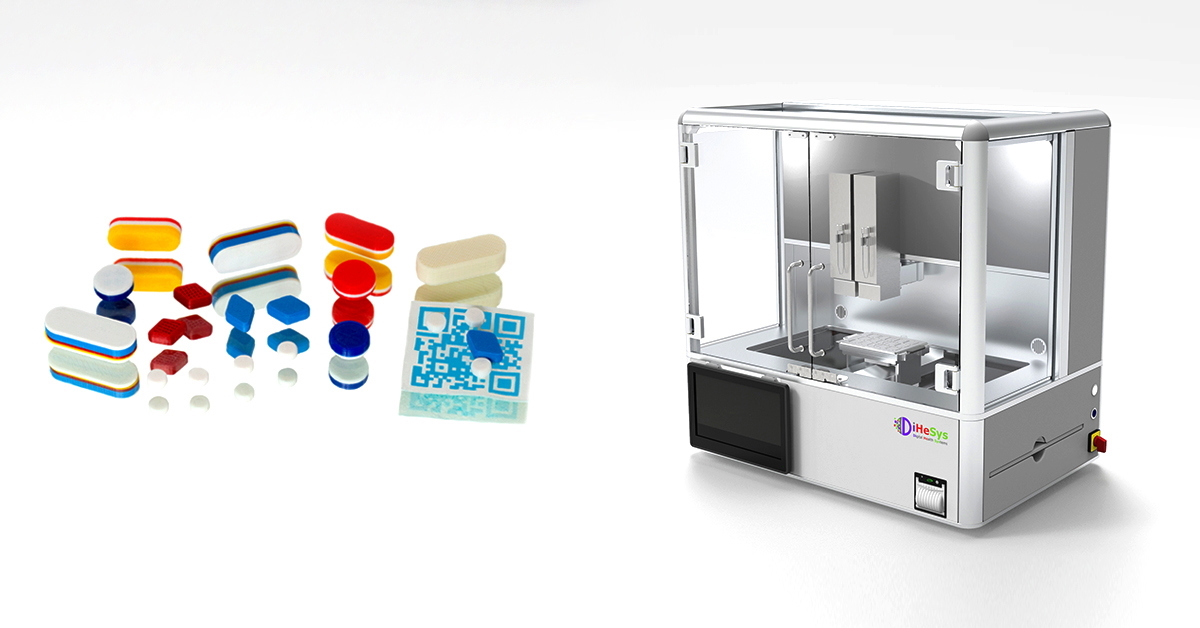
The start-up from Ulm entered into a strategic alliance with Harro Höfliger Verpackungsmaschinen GmbH from the city of Allmersbach im Tal (administrative district of Rems-Murr) in spring 2020. Harro Höfliger Verpackungsmaschinen is a global company in the field of pharmaceutical engineering. Working with Harro Höfliger’s engineers, DiHeSys is seeking to develop GMP-compliant dosing systems for 2D and 3D printing. The aim is to produce patient-specific thin films and tablets for widespread use in clinics and public pharmacies. Höfliger now holds an undisclosed financial stake in DiHeSys.
DiHeSys’ managing directors are convinced that doctors and pharmacists of the future will prescribe and produce individualised drugs. With the help of personal patient data such as weight, height and lifestyle habits, one idea is to produce drugs directly in the pharmacy. The partnership with Harro Höfliger also envisages providing a service to ensure the smooth running of on-site pharmaceutical printers and safe production without disruptions. The pharmaceutical printers will be sold under the DiHeSys label and target the global market.
So far, the two companies have developed the housing for the pharmaceutical printer, which can print both 2D and 3D. One print head is used for each active ingredient, after which the print heads and the cartridge containing either ink or filament are changed rather than being cleaned, which would be unacceptable under GMP conditions. Depending on the size of the pharmacy or the scope of care, a larger (currently equipped with up to four print heads) or smaller printer housing can be used. For larger manufacturing pharmacies that supply hospitals, for example, several printer housings could be installed and there are also plans to develop printers with space for a larger number of print heads.
3D printing for higher drug loading
Franken, who holds a PhD in pharmaceutics, believes that 80 percent of all currently available drugs are 'printable', pointing to numerous studies that have shown this is the case. The remaining 20 percent are 'injectables'. According to a review article by DiHeSys and GenPlus authors1, 2D printing technology is suitable for low-dose active ingredients (currently a maximum of 40 mg of active ingredient) and small pill quantities. Several active pharmaceutical ingredients with different release kinetics can be combined in one tablet (polypill) with 3D printing technology (mainly the fused deposition modelling process). According to experts, 3D printing processes are better suited for combining greater amounts of active pharmaceutical ingredients in tablets than two-dimensional ones.
At the moment, it is difficult to assess which paths individualised pharmaceutical printing will take in changing healthcare markets as they undergo digital transformation. As a provider of systemic services, DiHeSys foresees different business models being applied as clients would vary from pharmaceutical companies and university hospitals, where pharmaceutical printers create clinical test samples to, depending on the location, on-site pharmacies, hospitals, compounding centres, manufacturing pharmacies and manufacturing centres.
Digitalisation in drug production has been a research topic in university institutes for years. However, only a few pharmaceutical companies and small start-ups (at least they do not so publicly) such as Merck in Darmstadt or the University College London start-up FabRx and Ulm-based DiHeSys are taking the next step towards the application of digitalised drug production.
First steps into application

As important as it is to drive forward the technological advancement of pharmaceutical printers, it is equally important to find active ingredients and indications that could have significant added value, i.e. clinical benefit, for patients.
According to the pharmacist Clive Roberts from the University of Nottingham, the anti-epilepsy drug Spirtam was the first 3D-printed drug approved by the US regulatory authority in 2015 because it solved a clinical problem related to swallowing disorders in young and older epilepsy patients: it provided a way to produce the drug with the new manufacturing technology so that it dissolved quickly in very little liquid2.
A pilot project that DiHeSys started in Tübingen in early summer 2020 is taking a step towards clinical application by focusing on testing the production of personalised drugs using digital printing. The project has a runtime of two years and is funded by the Baden-Württemberg Ministry of Economic Affairs, Labour and Housing as part of the Baden-Württemberg Health Region Forum.
Pilot project in Tübingen creates the basis for clinical studies
The project involves the University and the University Hospital of Tübingen. Prof. Dr. Stefan Lauter, director of the Institute of Pharmacy, emphasises the pilot character of the project, aimed at creating the prerequisites for later clinical studies. New dosage forms first need to be developed for digital pharmaceutical printing. According to the pharmacist, the long-term goal is the treatment of a patient for a specific indication (malignant brain tumour). The scientists have chosen protein kinase inhibitors to find out whether active pharmaceutical ingredients are suitable for digital printing. The idea is to ascertain whether these drugs, which are primarily used in tumour therapy and have to be administered on a highly individual basis because of their side effects, could be produced using 2D or 3D printing.
The researcher from Tübingen is at pains to emphasise that this is the early development stage of the project. It is highly unlikely that brain tumour patients will be treated as part of the project. The researchers chose malignant brain tumours as an indication as there is currently no adequate therapy available, although there may be active pharmaceutical ingredients, which, however, cannot be individualised. The pilot project aims to find an answer to the question as to how a mass type of medication such as pills can be turned into an individualised dosage form.
Technology must deliver what it promises
Laufer explains the next steps: the Tübingen pharmacists will initially produce many solution formulations for the protein kinase inhibitors, test these solvents for compatibility with 2D/3D printing technology, and then start searching for polymers that are suitable for digitally printing a matrix. The project partners are hoping that the final result will be a drug with a solution combination of one or two matrices, for which model 2D or 3D prints can be produced. These prints will then be examined to find out whether they can be used for patients. The initial focus will be kinetics studies. If the pilot project is successful, as Laufer expects, then the project will come up with a drug in combination with one or two different matrices for 2D or 3D printing with good kinetics.
It is also clear that this technology can only be used for diseases for which specific individual therapies are available, i.e. for more serious diseases of vital interest. Laufer hopes that initial results will be available by the end of the first quarter/beginning of the second quarter of 2021. It is already possible to use this technology, but only for a limited number of drugs and matrices - the Tübingen pilot project also aims to broaden the use of the technology. It has proven its feasibility, now it needs to be applied.
References:
1) Dachtler, Markus, Huber, Gerald, Pries, Tanja: 2D- & 3D-Print-Technologien in der pharmazeutischen Industrie, Wiesbaden 2020. In: Pfannstiel, M.A., Da-Cruz, P., Rederer, E.: Digitale Transformation von Dienstleistungen im Gesundheitswesen VII, p. 53-66, DOI:10.1007/978-3-658-26670-7_4.
2) Andrew Tunnicliffe: The past, present and future of 3D printing in the pharmaceutical industry. In: World Pharmaceutical Frontiers 09 Mar 2020 https://www.ns-healthcare.com/analysis/additive-manufacturing-3d-printing/