Project BlindZero
Hope for patients with eye diseases: human cornea from 3D printers
Thousands of cornea transplants are performed every year in Germany. However, donors are rare and the procedure is not always without complications. Researchers at the University of Heidelberg are now developing an innovative technique in a project called BlindZero. It involves ‘printing’ human corneas directly onto patients’ eyes using 3D bioprinting. The reprogrammed genetically engineered cells used for this purpose are not expected to cause a rejection reaction.
The cornea is the transparent front part of the eye that accounts for most light refraction and forms the first protective barrier in the eye. If this barrier is damaged due to injury, infection or hereditary defects, and the damage cannot be treated with eye drops, antibiotics or anti-inflammatory drugs, the only option to prevent severe vision problems that can lead to complete blindness is a donor tissue transplant.
Cornea transplants are performed around 9,000 times a year in Germany alone.1) However, there are long waiting lists because demand for donor tissue is significantly higher than the number of cornea donations, and the procedure itself is not without risk. Despite considerable progress in surgical techniques, rejection reactions can occur, for example, when the patient's immune system rejects the foreign tissue. This is common to all transplants involving foreign tissue.
Bio-ink made from corneal cells and hydrogel printed with the 3D printer
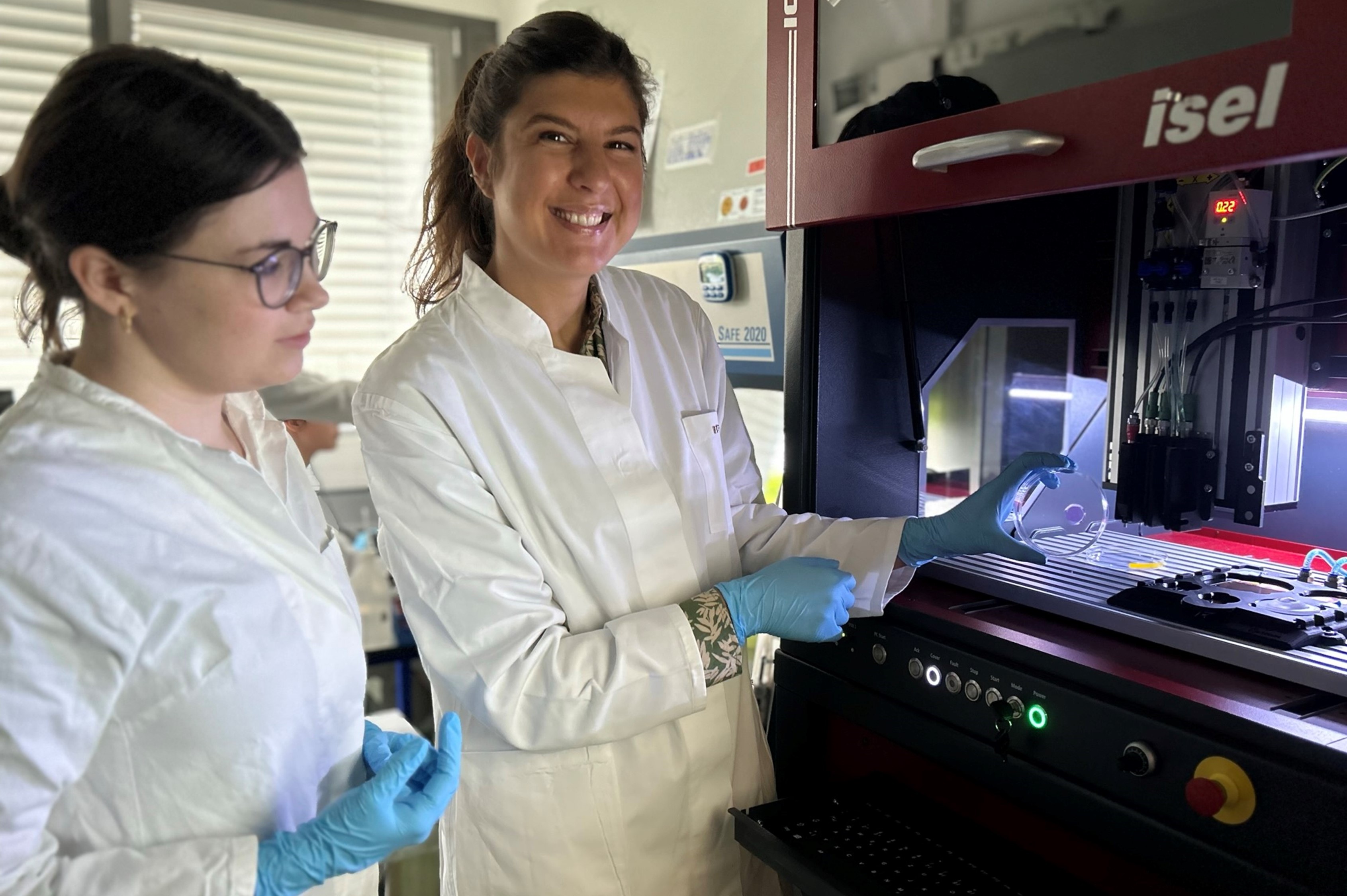 Dr. Friederike Dehli (left) and junior professor Dr. Daniela Duarte Campos (right) and their team at Heidelberg University are developing a cornea from human cells that will one day be produced by a 3D printer in the operating theatre. © University of Heidelberg
Dr. Friederike Dehli (left) and junior professor Dr. Daniela Duarte Campos (right) and their team at Heidelberg University are developing a cornea from human cells that will one day be produced by a 3D printer in the operating theatre. © University of HeidelbergAn alternative from the laboratory that could restore vision in a timely manner would be a blessing for people suffering from irreversible corneal diseases that cannot be treated conventionally. Researchers in the Bioprinting & Tissue Engineering junior research group at Heidelberg University’s Centre for Molecular Biology have been working for some time on technologies and biomaterials for tissue and organ engineering, including 3D printing methods and bio-inks for producing human corneas. Initial tests of possible materials and methods have already proved very promising.
The BMBF has awarded a grant of almost 2.2 million euros over a period of five years to the BlindZero project led by junior professor Dr. Daniela Duarte Campos. The researchers' idea is to create a new cornea by mixing living human cells with a cross-linkable polymer solution to create bio-ink that can be ‘printed’ directly onto the patient's eye using a 3D printer. "BlindZero’s goal is to develop a kind of ‘ready-made tissue’ so patients can be treated at an early stage. Our tissue will consist of human corneal cells that do not necessarily have to come from the patients themselves. Therefore, there would no longer be a long wait for the corneal cells to be cultivated," explains Duarte Campos. "Ideally, we hope this solution can be used to treat eye diseases without having to rely on donor tissue."
Cross-linking tissue with the help of natural substances and visible light
To produce the innovative transplants, human corneal cells are multiplied by cell culture and mixed with a polymer solution. The solution cross-links, forming hydrophilic, three-dimensional polymer networks known as hydrogels. Due to their high water content, these hydrogels are particularly suited to tissue engineering (the artificial cultivation of tissue). "We have already tested hydrogels available on the market but we will also work on new formulations," the scientist says. "We have a number of different options available: there are both natural and synthetic polymers, which can be crosslinked to form corresponding hydrogels. We can also adjust the viscosity of the bio-ink to ensure the best possible printing process."
Intensive research is also being carried out on the polymerisation process. "There are just as many possibilities here," says the junior professor. "But our focus is on using visible light for the cross-linking process in which a photoinitiator triggers polymerisation. It goes without saying that the ‘artificial’ cornea must not be toxic to the body and cells over both the short and long term. So this will have to be studied in detail. However, initial in vitro tests have shown that cells survived without damage. We are now concentrating primarily on natural substances that do not harm the environment or the body."
Individual printing process as close to the eye as possible
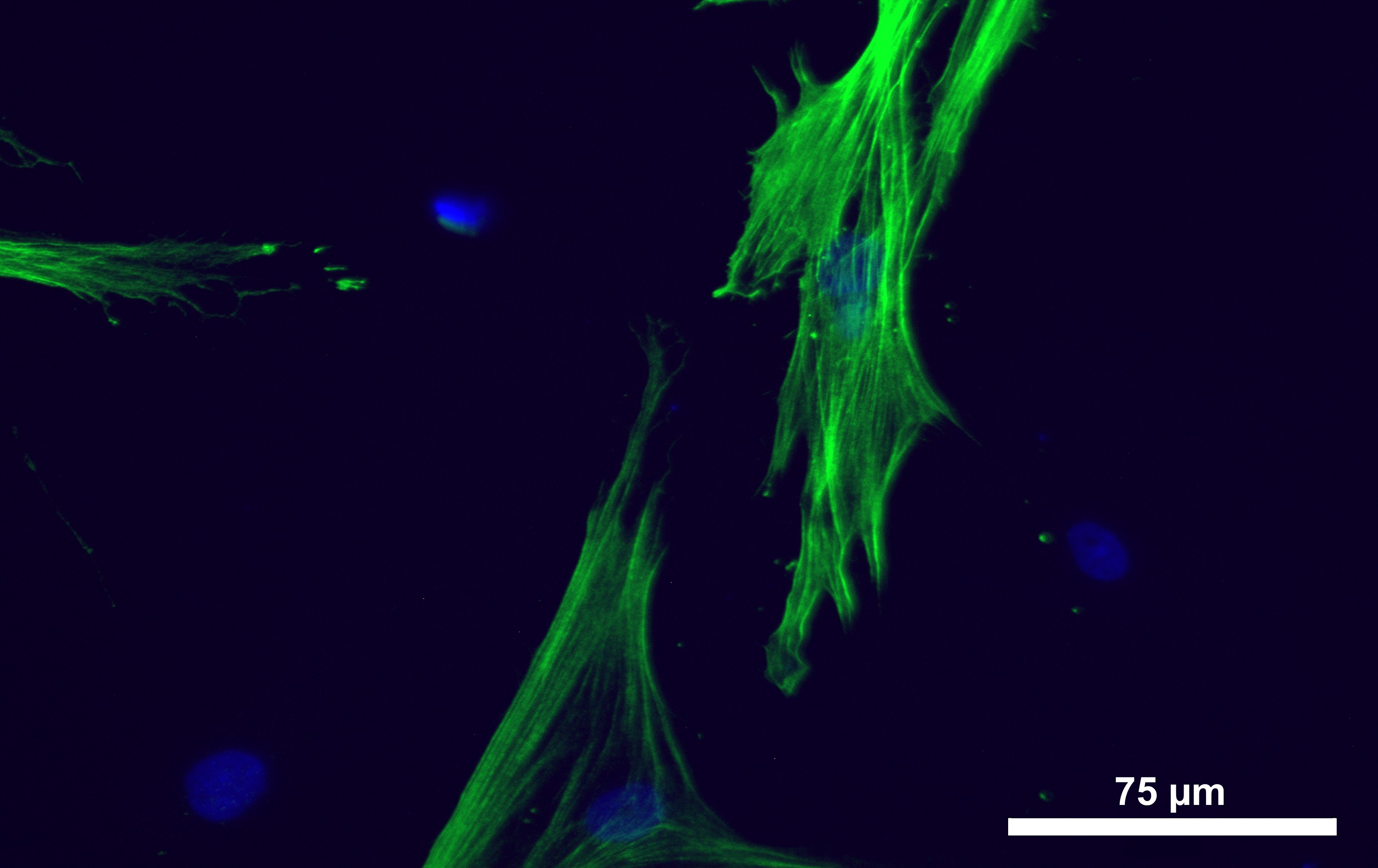 Keratocytes (corneal cells derived from mesenchymal stromal cells cultured in vitro for a fortnight showing positive staining (green) for the enzyme ALDH3A1(aldehyde dehydrogenase 3 family member A1) - a characteristic marker for human corneal cells. © University of Heidelberg
Keratocytes (corneal cells derived from mesenchymal stromal cells cultured in vitro for a fortnight showing positive staining (green) for the enzyme ALDH3A1(aldehyde dehydrogenase 3 family member A1) - a characteristic marker for human corneal cells. © University of HeidelbergThe specially cultivated cell-polymer mixture is subsequently loaded as a bio-ink into a 3D printer, where a new patient-specific cornea is printed layer by layer. The idea is to apply this mixture directly to the patient’s eye in a single surgical intervention and thus generate a new cornea. "Printing is the second area we are specifically focused on," Duarte Campos says. "In addition to searching for optimal hydrogels and formulations, we are working hard to develop the printing technology that will allow us to shape the living cells into tissue. At the moment, we are testing a bioprinter that produces very small bio-ink droplets, which, in contrast to the most common method at the moment - extrusion printing - organise themselves into the tissue through polymerisation after printing. There is still a lot of work to be done: for example, we want to make the process faster and even more precise, so that in future a robotic arm will be able to do this on a very small scale within a few micrometres of the patient's eye in the operating theatre – as close to the patient’s eye as possible." The researchers are also working on an interactive monitoring system consisting of a camera and sensors, which will enable individual adjustments during the printing process in real time.
The ultimate goal is a fully automated procedure. "Utmost care must be taken to mix the corneal cells with the polymer solution in order to avoid mechanical stress so that as many cells as possible survive," explains Duarte Campos. "A pipetting robot could do that very reliably. And it would also be possible to combine the different procedures, such as transferring the bio-ink into the printer cartridge, which would make the process as efficient as possible and reduce the potential for error."
Avoiding rejection reactions by tissue engineering
Further intensive research will also be carried out on transplant rejection. "This involves us working with the university eye hospitals in Heidelberg and Aachen," says the expert. "Extensive tests will be carried out with immortalised and primary cells from a human cornea bank. For the envisaged solution, iPSCs (induced pluripotent stem cells) will then be used, as ideally they will prevent immune reactions."
Work on BlindZero began in early 2022. The team of researchers was put together and practical work on developing the corneal tissue has now been going on for around six months. The researchers expect to have developed the technology and material within two to three years. This includes testing on animal eyes from abattoirs, followed by preclinical tests. The researchers hope to start applying for the clinical trial phases by the end of the five-year project period.
Info box: The BlindZero project
Title: "In vivo bioprinting keratoplasty with biocompatible, natural bionics, that crosslinks under visible light"
Project duration: 2022 to 2026
Participating institutions: Centre for Molecular Biology, University of Heidelberg and '3D Matter Made to Order' cluster of excellence of the University of Heidelberg and the Karlsruhe Institute of Technology (KIT)
Industry mentors and project partners: Black Drop Biodrucker GmbH, Fibrothelium GmbH, PL BioScience GmbH
Funding reference: 13XP5135