Biochip systems
Miniature organs with great potential
Junior professor Dr. Peter Loskill and his team at the Fraunhofer Institute in Stuttgart and the University Hospital of Tübingen are developing what is known as an "Organ-on-a-Chip" (OoC). An OoC is a microfluidic system that simulates small functional units of organ tissue. OoCs can be used in many different ways - in basic and pharmaceutical research as well as in clinical research and application, where they might in future render many animal experiments superfluous. The small chips are also being used in the search for active pharmaceutical ingredients to combat the novel coronavirus.
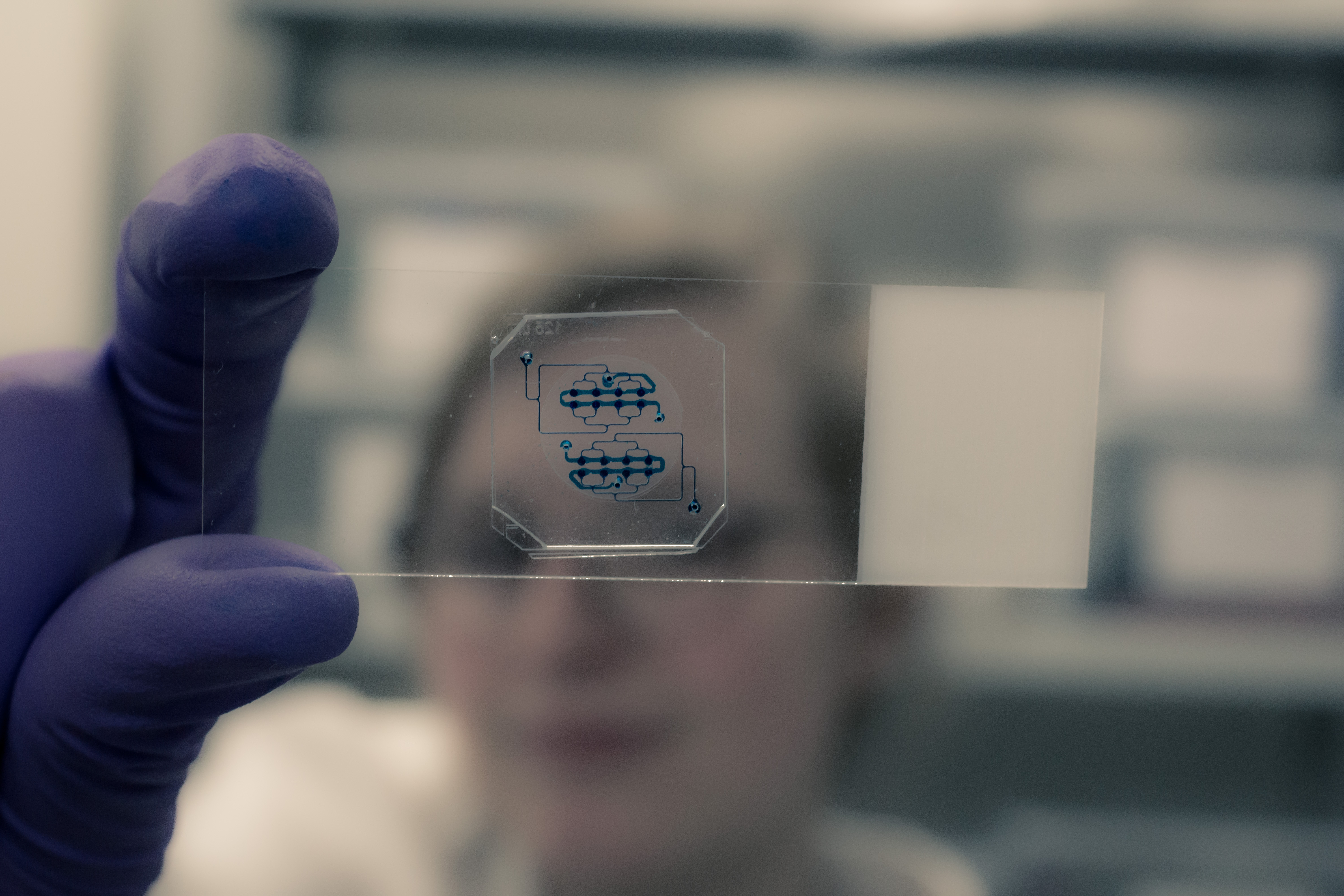 Structure of an Organ-on-a-Chip - the capillaries and chambers running through the chip are clearly visible. © Fraunhofer IGB
Structure of an Organ-on-a-Chip - the capillaries and chambers running through the chip are clearly visible. © Fraunhofer IGBOn average, it takes over ten years before a new drug is ready for the market - an active pharmaceutical ingredient has to go through numerous development phases before it is market-ready. Before it can be tested on humans, its safety and efficacy are first tested in detail in laboratory tests (preclinical studies). Manufacturers have not yet been able to avoid animal testing in this phase of drug development. Although animal experiments are strictly regulated in Germany, the subject is still a highly controversial issue and the clamour for alternatives is loud.
Besides ethical concerns, there are also very practical reasons why alternative systems to animal experiments are needed for preclinical drug development: on the one hand, the transfer of findings from preclinical to clinical application - so-called translation - often fails due to a lack of efficacy, toxic reactions or other undesired effects in humans. On the other hand, some drugs show undesired reactions in animal models even though they pose no risk to humans. Laboratory results and animal experiments cannot therefore be easily transferred to humans. Many test substances fail in late development phases, and this can cost manufacturers millions.
Organs-on-a-Chip (OoCs) are microfluidic plastic chips that use mechanical and biochemical elements to mimic small functional organ units after the application of tissue cells.
Organs on chips have the potential to replace many animal experiments
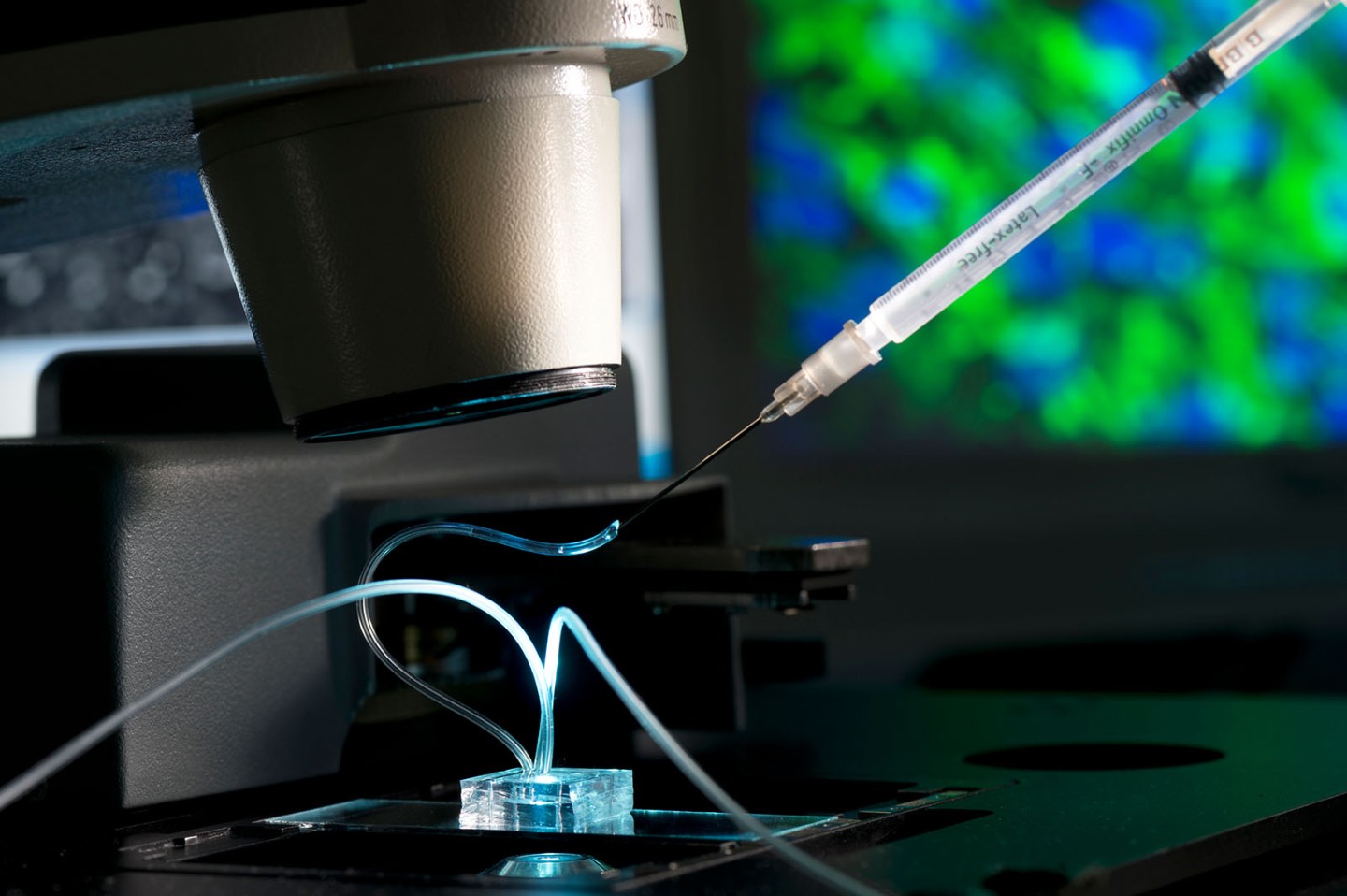 Fat chip under the microscope: with the help of a syringe, an active substance is applied to examine its effects on the fat cells. © Fraunhofer IGB
Fat chip under the microscope: with the help of a syringe, an active substance is applied to examine its effects on the fat cells. © Fraunhofer IGBDr. Peter Loskill, head of the Innovation Field Cell and Tissue Technologies at the Fraunhofer Institute for Interfacial Engineering and Biotechnology IGB in Stuttgart and junior professor at the University of Tübingen, and his team have been working for many years on the development of systems that imitate the structure and functionality of organ tissues on a small area. These Organ-on-a-Chip systems are an excellent prospect for simulating complex physiological processes in humans and might in future render some animal experiments superfluous. "These systems alone will not completely replace animal experiments in drug development," Loskill emphasises, "but we will be able to reduce the numbers of such experiments significantly."
The chips are three-dimensional microfluidic systems with tiny chambers and channels that, due to their mechanical, geometric and biochemical properties, mimic the microconditions in human tissue. By introducing cells into this environment, it is possible to create coherent tissue. "Of course, we cannot reproduce entire organs on a chip, but we can reproduce small functional units of organs," explains Loskill. The channels in the chip mimic blood vessels through which nutrients or test substances such as new drugs can be flushed.
In clinical research, the chips could give indications as to how a particular patient would react to a particular therapy. At the University Hospital in Tübingen, Loskill is working with Dr. André Koch and Prof. Dr. Sara Brucker to simulate tumour microenvironments in 3D models of this kind in order to subsequently introduce breast cancer tissue from female patients. They will then test the individual reaction of the breast cancer models to different cancer drugs. "If this approach proves successful, we will be much closer to the goal of individualised and customised cancer therapy," said Loskill.
Broad field of application - not only in drug development
The small organ units that are replicated on OoCs are not only used in clinical applications, but also in basic research and pharmacological research. Fields of application include:
Gaining a better understanding of the function of fat tissue
In a healthy person, fat tissue represents around 25 percent of the human body, in an obese person it can be up to 50 percent. Fat tissue therefore makes up a considerable proportion of a person’s total tissue. However, its importance has not yet been investigated thoroughly. Loskill and his team have developed what they call "WAT-on-a-chip". (WAT stands for "white adipose tissue") in order to better understand the importance of adipose tissue and be able to draw conclusions on diseases such as obesity or diabetes. The scientists are using this chip to investigate the physiological properties of fat, i.e. adipose tissue and gain a better understanding of processes such as substance storage.
Testing active pharmaceutical ingredients against COVID-19 in the lung model
In June 2020, Loskill's team and partners from the Fraunhofer Society launched the "Fraunhofer vs. Corona" project: using the "lung-on-a-chip" platform, the scientists intend to test already approved drugs for their pharmacological effect against SARS-CoV-2. The chip represents an infection model that simulates the pathogenesis of COVID-19. It will be made available to companies interested in testing their own active pharmaceutical ingredients.
Teaching organ models to see
Another new and exciting approach from the Loskill laboratory is what the researchers call "retina-on-a-chip". This microfluidic chip simulates the human retina. In cooperation with Prof. Stefan Liebau's Institute of Neuroanatomy and Developmental Biology at the University Hospital in Tübingen, Loskill and his team have produced tissue from stem cells, including light-sensitive rods and cones, the pigment epithelium and ganglion cells that form the optic nerve. They are currently in the process of "teaching the retina to see". Following exposure to light, they were able to measure an electrophysiological signal - a sign that signal transmission on the chip works in a similar way to the nerves of the human eye. "The retina-on-a-chip system is particularly interesting for pharmaceutical manufacturers", says Loskill. Pharmaceutical companies can use the chip to study whether active pharmaceutical ingredients cause undesired side effects in the retina.
An Organ-on-a-Chip may be small but its possible applications are diverse and the potential of the models is huge - in research as well as in development. If it is possible to adapt physiological conditions as accurately as possible to the complex conditions in vivo, the miniature organ models will soon represent valuable alternatives to animal experiments, facilitate pharmacological and clinical studies and save huge amounts of money in drug development.