Whole blood model enables development of early warning system for sepsis
Sepsis is a life-threatening disease that can be treated all the more successfully the faster therapy is initiated. It is not just the infection itself that is so dangerous, but a dysregulated response of the immune system. Physicians at Ulm University Hospital have now developed an animal-free test system that can be used to research the disease and develop innovative diagnostic tools to quickly assess a patient's sepsis risk and optimise treatment.
Sepsis - otherwise known as blood poisoning - is a life-threatening condition caused by a reaction to a wide variety of infections. It is triggered by the uncontrolled multiplication of viruses, bacteria or fungi in the blood. For a long time, the pathogens themselves were considered the cause of the disease. However, since 2016, sepsis has been redefined as an excessive and dysregulated response of the immune system, which is then no longer able to fight off foreign pathogens entering the body, and also leads to multi-organ failure1. Worldwide, around 50 million people are diagnosed with sepsis every year2, and the numbers are rising, partly but not exclusively due to the coronavirus pandemic.
The faster a clear diagnosis can be made, the more successfully a disease can be treated. For this purpose, it is common practice to detect pathogens microbiologically as well as to record the response of the immune system with biomarkers. However, these analyses can take several hours to days.
Whole blood model simulates inflammatory reaction in sepsis
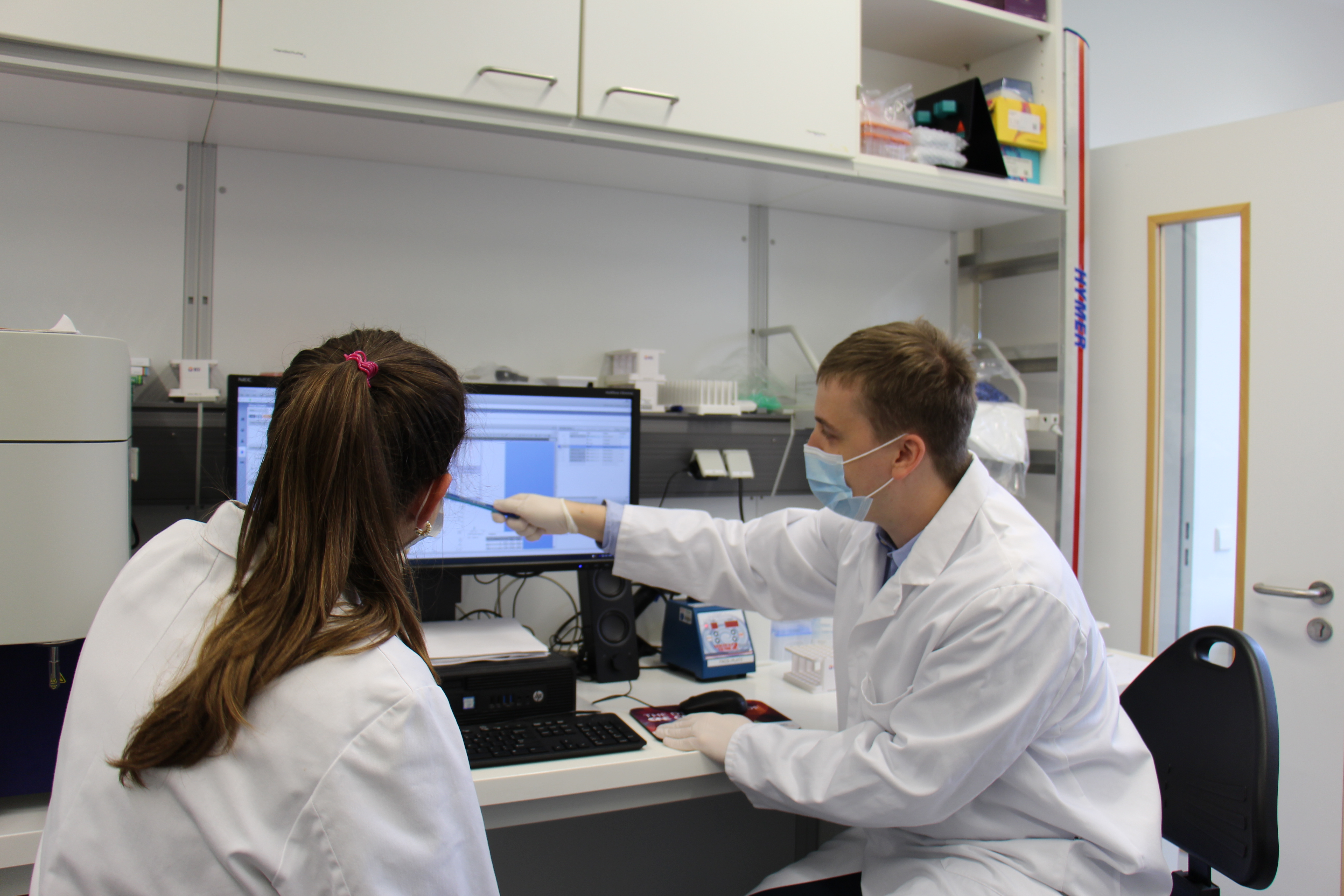 Dr. David Messerer and his team have developed the sepsis model. © Ulm University Hospital
Dr. David Messerer and his team have developed the sepsis model. © Ulm University HospitalDr. med. David Messerer, physician and head of the Immunomonitoring working group at the Institute of Clinical and Experimental Trauma Immunology at Ulm University Hospital, believes there is urgent need for action. This is why Messerer and his team set themselves the task some time ago of researching the molecular processes of sepsis and looking at how an individual patient’s risk of developing sepsis could be assessed within the shortest possible time - for example with the help of early markers for an excessive immune response. In this way, patients could be stratified very quickly and the attending physician could better decide the intensity of treatment required.
The researchers’ research had a successful outcome. Messerer and his colleagues recently presented a whole blood model for research and future diagnostic purposes that realistically simulates the inflammatory response in sepsis, but does not involve any additional stress or risk for the patient3. Previous alternatives required animal models, which for ethical reasons can only be used to a very limited extent and are not optimally suited to solving all questions. "Mice and pigs are not human beings," explains Messerer. "Animal experiments often provide clinically relevant data, but which cannot always be fully transferred to the situation in humans."
Stable conditions as in venous blood
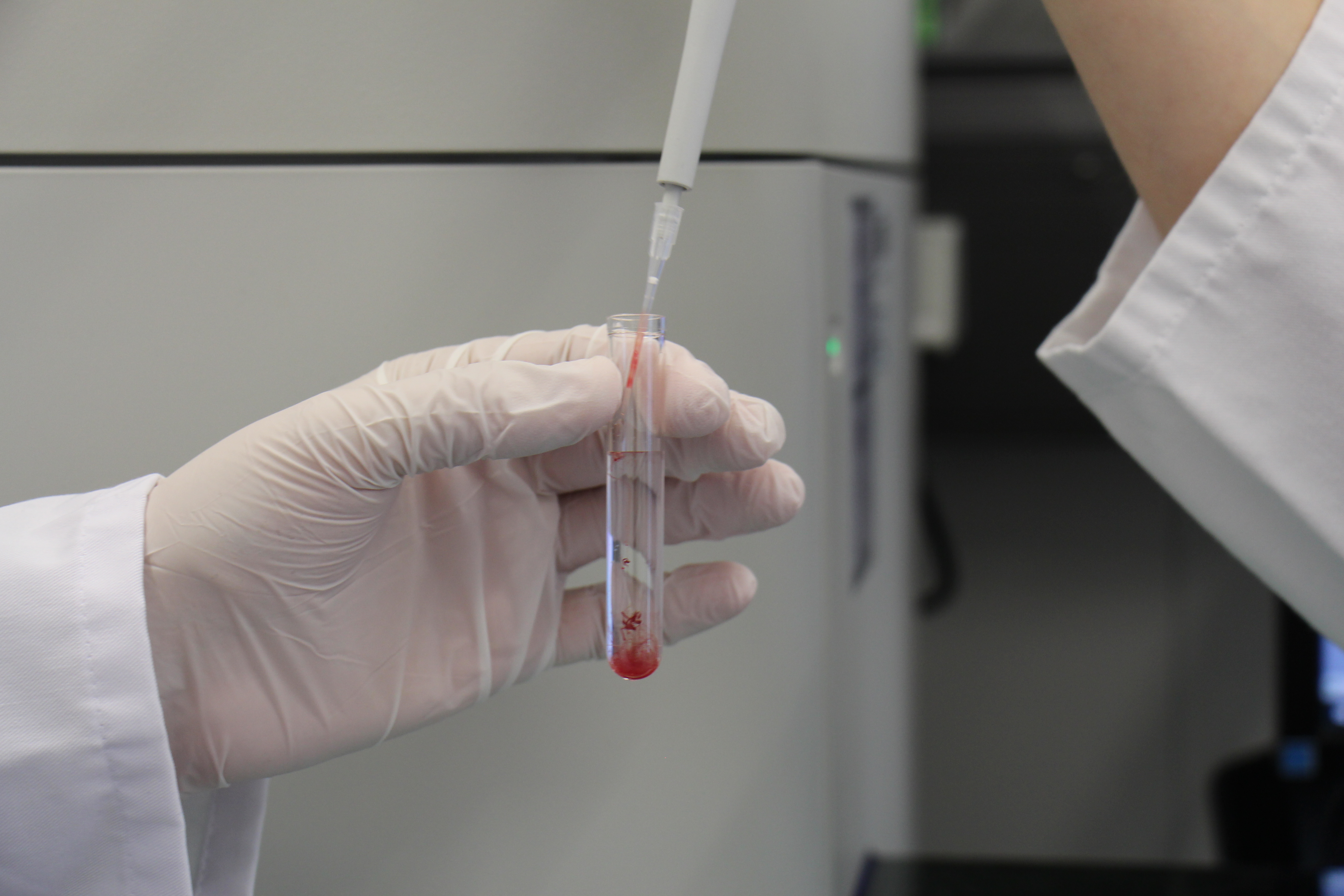 Only a few millilitres of blood are required for examination. © Ulm University Hospital
Only a few millilitres of blood are required for examination. © Ulm University HospitalThe novel sepsis model developed by the Ulm researchers involves adding bacterial components or whole pathogens to a blood sample and simulating the inflammatory response in the blood as sepsis develops. Special methods for treating the blood allow it to be used outside the body without clotting. "This was not previously possible," Messerer reports. "Now you can safely withdraw a few millilitres of blood and realistically study the inflammatory response of the human immune system to an infection. And do so without using animal experiments. We are particularly interested in immune system changes and subsequently, of course, how we can counteract these changes medically. Another advantage of the model is that we can safely test the behaviour of immune cells to new drugs. One limitation is that this is currently an organ-free system, so in future we will also have to validate our results using cell cultures and artificial organs."
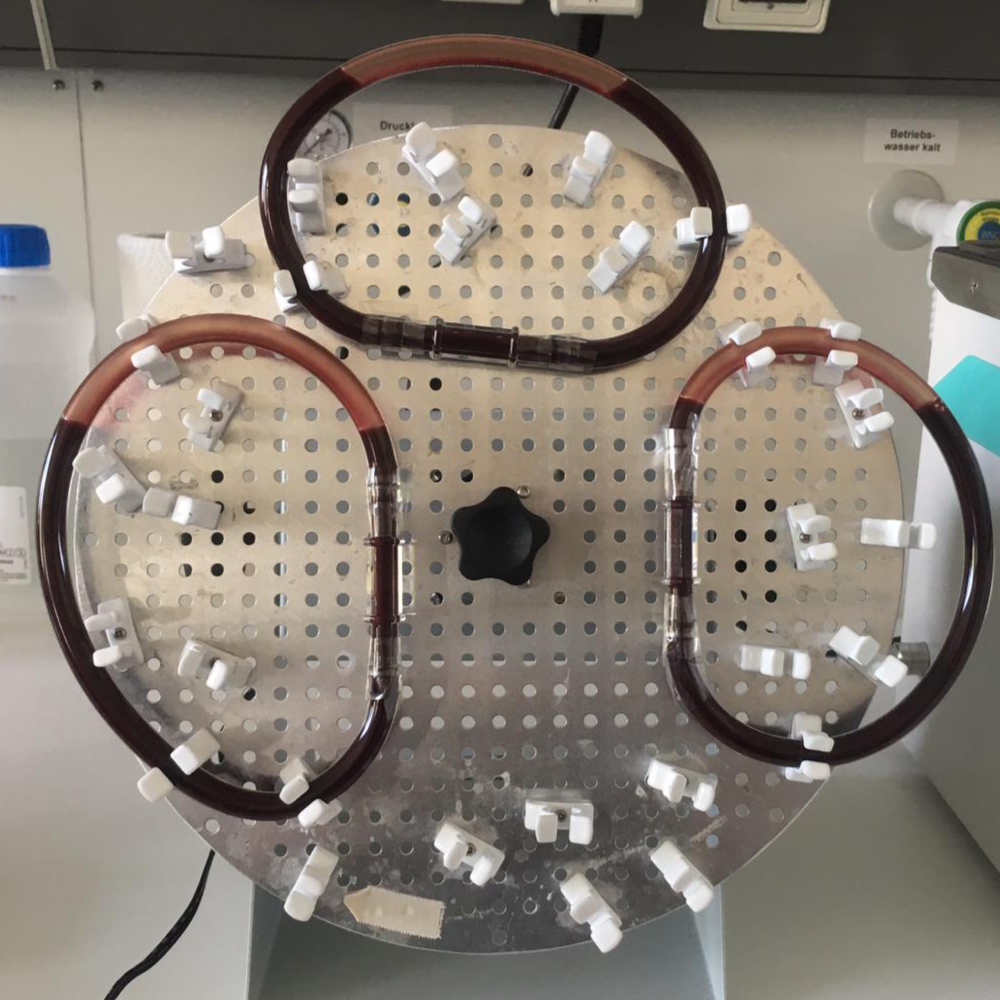 In the tubing system created by the Ulm researchers, a blood sample can be examined for essential sepsis parameters quickly and under realistic conditions. © Ulm University Hospital
In the tubing system created by the Ulm researchers, a blood sample can be examined for essential sepsis parameters quickly and under realistic conditions. © Ulm University HospitalThe core of the whole blood sepsis model is a continuously rotating air bubble that ensures continuous circulation and stability of the body fluid. "In this way, the blood in the model behaves very similarly to the venous part of the human body, where the immune cells are predominantly active," explains the researcher. "This was very important to us. However, there is a key difference between our model and the heart in that the latter pumps blood rhythmically rather than continuously. We decided against using a mechanical pump to simulate the rhythmic pumping of the human heart."
In this way, a whole blood sample can be examined for essential sepsis parameters within a very short time. Here, the focus is not on inflammatory molecules dissolved in the blood plasma, but on rapidly occurring immune cell changes. "This is a paradigm shift in sepsis diagnosis," explains institute director Prof. Dr. Markus Huber-Lang, who is closely involved with the project, "because we are now able to analyse the processes that take place in the cells. We do this by examining the blood sample with dyes, and measuring surface markers as well as pH. We are also looking at how white blood cells interact with the environment, which plays a role in organ damage. This has similarities to what we are also currently observing in COVID-19, where the immune system is massively active for hours and days against its own body. This so-called thromboinflammation leads to microclots and immune cell activation. Both can lead to multi-organ failure."
Easy-to-use diagnostic test for hospitals
However, the intention is not to keep the animal-free whole blood sepsis model in the laboratory for research purposes only. In future, the scientists want the system to be available for use in hospitals to determine the sepsis status of newly admitted patients in a matter of minutes or hours. "Around one in four ICU patients suffers from sepsis," says Messerer. "In ICUs, we can measure and monitor all organ functions 24/7, but we cannot do this with the immune system. Immune system parameters, such as the C-reactive protein (CRP value), have a delayed response time of 12 to 24 hours. This is too long. Our system measures whole cell processes rather than cellular end products. This is how we can significantly reduce the time required to visualise pathological changes."
According to the current state of research, the whole blood sepsis model would take just a few minutes to provide information as to whether there has been an excessive immune response to an inflammatory reaction, thus giving an initial assessment of a patient’s risk of developing sepsis. Based on this information, the decision could then be taken to either send the patient home again or admit them to the ICU without delay.
In addition, the model was used to study further criteria that could be used for an immune status test. "We are now validating the test on sepsis patients," says the expert. "The test contains about 50 parameters for immune cells and blood platelets. The final step will be making the procedure simple enough to use as a solution for every medium-sized hospital rather than limiting it to trained laboratory employees only. Ideally, it would be a case of putting a drop of blood into a reaction vessel, placing the latter into a suitable analyser, pressing the start button and obtaining the valid result within thirty minutes."
Clinical trials in the pipeline
Once the coronavirus pandemic subsides, the researchers want to begin clinically validating the model on sepsis patients. In addition, the test will be optimised so it has fewer parameters and is even faster. If successful, the goal is to confirm the results with other clinical and laboratory partners in a multicentre study. The use of the test for COVID-19 would also be a highly interesting option, says Messerer, pointing out however that this will remain on the backburner for the time being so as not to disrupt ongoing studies.
The development of the model was supported by the Institute for Trauma Immunology and the Clinician Scientist Programme of the Medical Faculty of the University of Ulm for research physicians. The project also received funding from the Baden-Württemberg Ministry of Science, Research through the Forum Health Region Baden-Württemberg.