Brain tumour patients could benefit from heavy ion therapy
Glioblastoma is a malignant brain tumour. It does not respond anywhere near as well to conventional forms of therapy than other tumours because it contains particularly resistant cancer cells. Scientists at the Heidelberg Ion Beam Therapy Center (HIT) at Heidelberg University Hospital and the German Cancer Research Center have shown that heavy ion therapy is effective against these cells.
 Prof. Dr. med. Dr. rer. nat. Jürgen Debus, Scientific and Medical Director of the Ion Beam Therapy Center in Heidelberg (HIT) © Heidelberg University Hospital
Prof. Dr. med. Dr. rer. nat. Jürgen Debus, Scientific and Medical Director of the Ion Beam Therapy Center in Heidelberg (HIT) © Heidelberg University HospitalGlioblastoma is the most common malignant brain tumour in adults. It belongs to the type of brain cancers known as gliomas, which develop from so-called glial cells, i.e. cells that support the nerve tissue in the brain. Statistically, glioblastomas are relatively rare. Around 4,500 glioblastomas were diagnosed in Germany in 2014, which accounts for around one percent of all new cancer cases. The disease can occur at any age. "We have very young patients between two and three years old and people up to the age of 90," says Prof. Dr. med. Dr. rer. nat. Jürgen Debus, scientific and medical director of the Heidelberg Ion Beam Therapy Center (HIT) at Heidelberg University Hospital.
Without treatment, the mean survival rate following diagnosis is three to four months. The mean survival rate indicates how long 50 out of 100 patients survive following diagnosis. "Mean glioblastoma survival rate is 18 months using standard forms of therapy," says Debus. "But it is difficult to speak in probabilities. Therapy has improved in recent years, especially in molecularly defined subgroups, so some patients survive for two to three years after diagnosis and are considered long-term survivors." Age plays a major role in survival: younger patients generally survive longer than older ones. Glioblastoma is basically incurable and over 90 percent of patients die of the disease within five years of diagnosis.
Tumour stem cells repair DNA damage
Today, glioblastoma is treated with combined therapy. Therapy starts with surgical removal of the tumour. Since individual tumour cells always migrate into the healthy tissue and cannot be removed, radiotherapy and chemotherapy will follow. "For a long time, the question was asked as to why brain tissue, which has only a limited regenerative potential, produces tumours that grow so aggressively," says Debus. Researchers now know that glioblastomas have cells with stem cell properties that repair damage and from which the tumour can regenerate itself over and over again.
Conventional radiation therapy uses X-rays or gamma rays, which consist of small packets of energy known as photons. Radiation therapy is most effective at a tissue depth of up to three centimetres. The radiation dose drops as the rays travel through the tissue. Inside the cells, the photons generate reactive oxygen molecules, which damage the genetic material of the cancer cells. In contrast to other tumours, glioblastoma reacts much less effectively to this type of radiation. This is because on the one hand, tumour stem cells can neutralise the reactive oxygen molecules and repair DNA damage. On the other hand, there is no oxygen in the poorly perfused interior of the tumour (hypoxia), leading to the formation of fewer reactive oxygen molecules, so that the hypoxic cells present are able to survive radiation. Tumour vessels and other tumour cells are destroyed by radiation, which leads to a kind of selection pressure. More hypoxic cells are then created, which also release substances that weaken the immune system.
Carbon ions are more biologically effective
 Radiotherapy room with rotatable (360°) radiation source, the so-called gantry. The ion beam can be directed onto the tumour from any direction. The HIT has two further treatment stations with fixed horizontal beam guidance. © Heidelberg University Hospital
Radiotherapy room with rotatable (360°) radiation source, the so-called gantry. The ion beam can be directed onto the tumour from any direction. The HIT has two further treatment stations with fixed horizontal beam guidance. © Heidelberg University HospitalHeavy ion therapy involves irradiating the tumour with positively charged nuclei of carbon, oxygen or helium atoms. The present study used cell cultures and mouse models to investigate how glioblastoma reacts to irradiation with carbon atoms. The charged particles were accelerated to over three quarters of the speed of light, thus covering approximately 225,000 kilometres per second. They can penetrate up to 30 centimetres deep into the tissue and are barely weakened, so that most of the energy is released on the tumour tissue. With this type of radiation, it is the carbon ions themselves that cause damage to the DNA. Tumour stem cells and hypoxic cells are unable to repair this damage. The destruction of the hypoxic cells also changes the tumour environment: the scientists were able to show that the composition of the immune system changes favourably and that, compared to conventional radiation therapy, fewer cells that weaken the immune system reach the tumour. Thus, glioblastoma could possibly also be made accessible to immunotherapies that have already been successfully applied for treating other tumours.
The symptoms of this malignant brain tumour are initially rather unspecific. "Symptoms include diffuse headaches, reduced performance, impaired memory or dizziness", says Debus. "The symptoms depend very much on where the glioblastoma is growing." A brain tumour can also lead to hemiplegia or epileptic seizures. There are no lifestyle habits or controllable risks that increase the likelihood of developing glioblastoma. "Glioblastoma patients haven’t done anything "wrong"," says Debus. There is only one factor that can be linked to the disease: therapeutic radiation treatment can slightly increase the risk of developing glioblastoma. "Two to three out of 100 patients that are exposed to higher therapeutic radiation doses develop a glioblastoma," says Debus. Statistically, it takes a long time for this risk to take effect. It is therefore particularly relevant for children and adolescents.
Research results to be transferred to patients
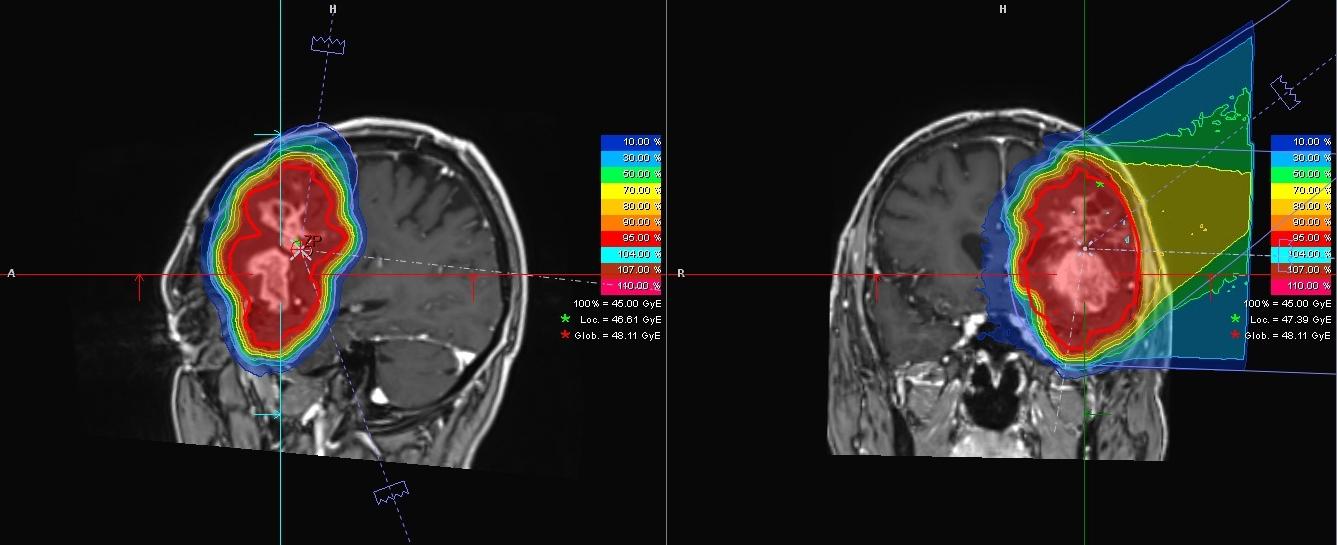 The images show the glioblastoma of a 55-year-old patient. The tumour, which is located near the left temple, was recorded from different perspectives with magnetic resonance imaging (MRI). The colours show the distribution of the planned radiation dose: it is highest in the area of the tumour (red), and becomes lower and lower the greater the distance to the tumour. © Heidelberg University Hospital
The images show the glioblastoma of a 55-year-old patient. The tumour, which is located near the left temple, was recorded from different perspectives with magnetic resonance imaging (MRI). The colours show the distribution of the planned radiation dose: it is highest in the area of the tumour (red), and becomes lower and lower the greater the distance to the tumour. © Heidelberg University HospitalHeavy ion therapy can also have undesirable side effects. This is because tumour tissue and healthy tissue are knitted together, without however impairing the function of the healthy tissue. "It is impressive," says Debus, "that patients who have a tumour in the language centre can often speak normally." In these cases, the healthy tissue might react to and be damaged by heavy ion therapy. "It is not possible to make a general statement," explains Debus. "In individual cases, however, it is possible to assess the likelihood of certain side effects."
The research results of studies on heavy ion therapy for the treatment of glioblastomas are based on cell cultures and mouse models. The team led by Debus is currently working on transferring these findings to patients. The first data from a study in relapse patients with high-grade gliomas are already available. A relapse is the recurrence of a tumour at the same place where the original tumour has been eliminated. "The first comparative studies of glioblastoma recurrence show a potential advantage of carbon ion therapy over photon therapy," reports Debus. "We will assess this in randomised prospective studies."