Peptide-based COVID-19 vaccine
CoVac-1: T-cell activator against COVID-19
Current vaccines against COVID-19 aim at forming neutralising antibodies that prevent the virus from penetrating the host cells. Since people with impaired B-cell immune responses – which can also occur in cancer or autoimmune diseases – are not able to do this, researchers at the University of Tübingen have developed the peptide-based T-cell activator CoVac-1, which promises broad and long-term immunity.
After contact with a pathogen, the defence cells of our adaptive immune system develop a tailor-made response so that in future it will be able to quickly identify and effectively eliminate the pathogen in question. B lymphocytes produce antibody molecules that recognise and bind foreign structures, so-called antigens, on the surface of the pathogen. The antibodies can thus block the infectivity of pathogens by preventing them from penetrating body cells, for example. Furthermore, when antibodies attach to antigens this acts as a signal for macrophages, which engulf and degrade the pathogen. This results in peptides that are bound to the MHC (major histocompatibility complex) protein complex and presented on the surface of the macrophages.
HLA molecules define the immunological self
With the help of the MHC protein complex, also called HLA (human leucocyte antigen) in humans, the immune system can distinguish between the body's own cells (self) and those of another individual (non-self) as well as recognise whether cells are infected or altered by a pathogen, for example. HLA class I molecules are found on all nucleated body cells. Since the associated genes are extremely variable, each person has an individual set of HLA class I molecules. They present short peptides (consisting of eight to ten amino acids) from all proteins that are synthesised inside the cell. If foreign proteins are produced as a result of an infection, cytotoxic CD8+ T lymphocytes detect their presence on the basis of the new peptides and destroy the corresponding cell.
Conversely, HLA class II complexes are predominantly formed by ‘professional’ antigen-presenting cells of the immune system, which include B lymphocytes and phagocytes. They present longer peptides that originate from ingested and digested proteins rather than from the cell's own material. These longer peptides are recognised by CD4+ T cells, which are primarily responsible for coordinating the immune response and support both B and T lymphocytes as well as phagocytes in combating the invader.
Long-lasting T-cell protection against COVID-19
 Prof. Dr Juliane Walz and her team are developing peptide-based T-cell activators that induce long-lasting immunity against SARS-CoV-2. © University Hospital Tübingen
Prof. Dr Juliane Walz and her team are developing peptide-based T-cell activators that induce long-lasting immunity against SARS-CoV-2. © University Hospital TübingenLike other viruses, SARS-CoV-2 invades and multiplies in host cells. Therefore, both the formation of antibodies and the activation of T cells are important for an effective immune response to occur. Common vaccines aim to induce neutralising antibodies that block the spike protein of the virus and thus prevent it from entering host cells. However, studies carried out on vaccinated individuals as well as individuals who have recovered from COVID-19 show that antibody levels decline after only a few weeks, whereas T-cell-mediated immunity lasts significantly longer. "In people who have recovered from SARS-CoV-2 infection, we have also seen that it is not necessarily the strength of the T-cell response that is decisive for a milder course of the disease, but the breadth, i.e. recognising many different peptides," explains Prof. Dr. Juliane Walz, head of the Department of Peptide-Based Immunotherapies and medical director of the Translational Immunology clinical cooperation unit (CCU) at the University Hospital of Tübingen. Walz is a specialist in internal medicine, haematology and oncology who usually works on the development of therapeutic tumour vaccines for treating malignant diseases.
Since the beginning of the coronavirus pandemic, Walz has been using her expertise acquired in cancer immunotherapy to produce a peptide-based vaccine against COVID-19 that induces long-lasting T-cell immunity. This is especially important for people who have a congenital or acquired B-cell defect and therefore either cannot produce antibodies or can only produce small amounts. This includes people with tumour diseases of the immune system (lymphomas, leukaemias), and patients who are immunosuppressed because they are receiving post-transplant treatment, for example, as well as people with autoimmune diseases.
CoVac-1 induces broad immunity
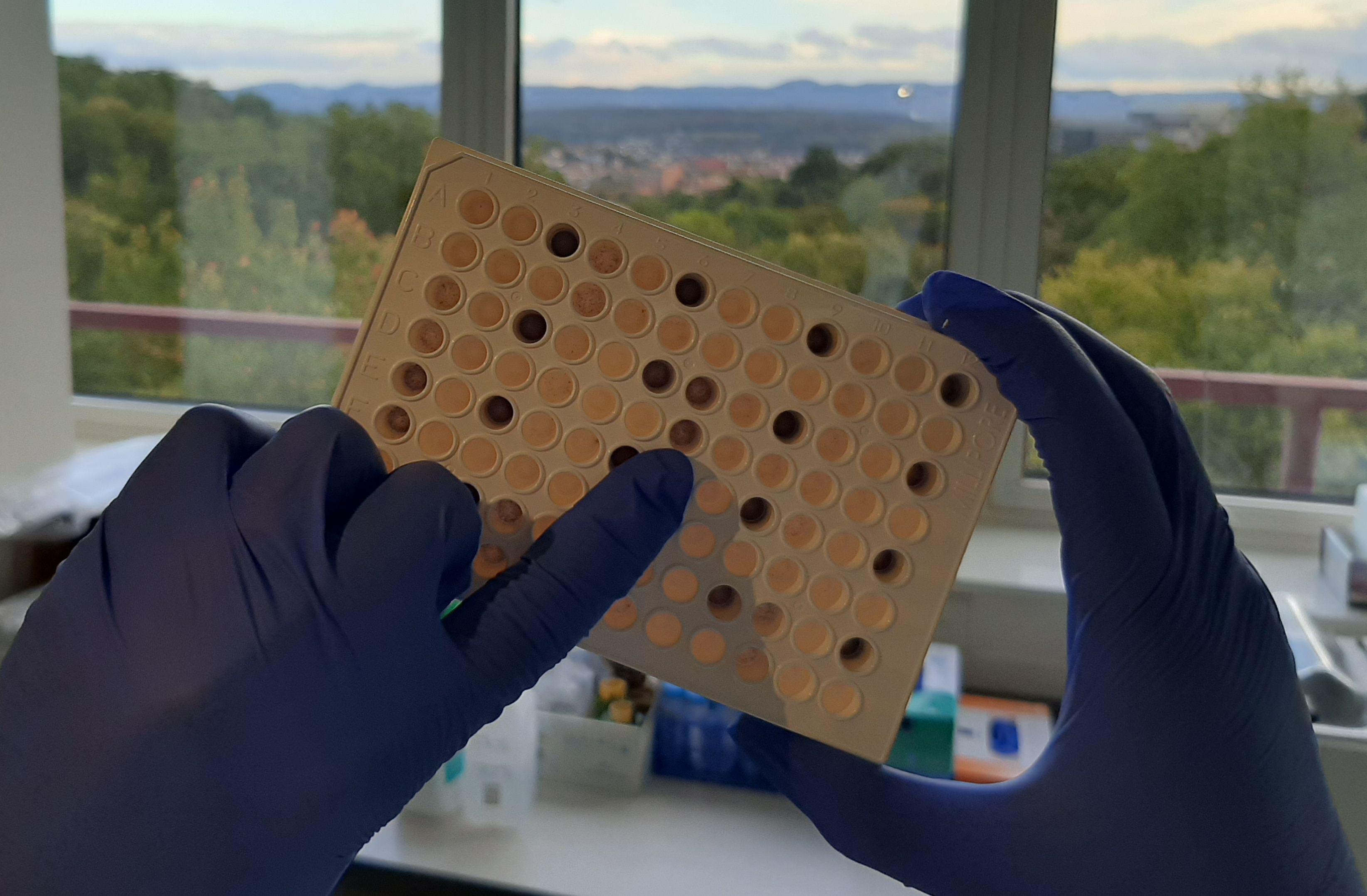 The so-called ELISpot assay can be used to identify peptides that are recognised by the T-cells of people who have recovered from the disease. © University Hospital Tübingen
The so-called ELISpot assay can be used to identify peptides that are recognised by the T-cells of people who have recovered from the disease. © University Hospital TübingenIn a first step, Walz's team identified peptides that elicited the strongest and most frequent T-cell responses, or a long-lasting response, in individuals who had recovered from the disease.1) These peptides originate not only from the spike protein but from all viral proteins and are presented either by HLA class I or class II molecules. Based on this initial information, the researchers developed CoVac-1. The multipeptide vaccine was developed in cooperation with the Department of Immunology of the Interfaculty Institute for Cell Biology at the University of Tübingen under the direction of Prof. Dr. Hans-Georg Rammensee.
CoVac-1 contains six long peptides whose sequences derive from four different viral proteins. "This peptide selection promises a broad immune response that is not hampered by mutations in the spike protein," Walz explains. "What's also special is that the long HLA class II peptides contain short sequences that can be presented by class I molecules, which should activate both types of T cells." These theoretical considerations were confirmed in a phase I clinical trial in healthy volunteers, which was successfully completed in summer 2021.2) In addition, CoVac-1 was shown to be very well tolerated and to elicit significantly stronger T-cell immunity (3 - 20-fold) after just one dose than common COVID-19 vaccines. Walz adds: "However, we now no longer see CoVac-1 as a vaccine, but as an additive T-cell activator that can be given to high-risk patients who have poor antibody protection, in addition to standard vaccination."
In a phase II clinical trial, which is already underway, CoVac-1 is being administered to a small group of immunosuppressed (e.g. leukaemia or lymphoma) patients. "Based on the encouraging data so far, we expect to achieve good results in this group of volunteers and therefore hope to be able to start a larger, pivotal study in the autumn," says Walz optimistically. For this purpose, the scientist is currently looking for a suitable industrial partner.
Many years of experience pay off
The rapid testing of CoVac-1 was only possible because of the University of Tübingen's many years of experience with therapeutic peptides. "We have a very special situation here in Tübingen in that the preclinical infrastructure for developing such vaccines is available alongside a ‘Wirkstofflabor’ where peptides are manufactured as active pharmaceutical ingredients (API) or drug substances (DS) according to GMP guidelines," Walz explains. "The Translational Immunology clinical cooperation unit headed up by Prof. Dr. Helmut Salih also gives us a department that has the facilities to translate self-developed immunotherapies into the clinic." All the institutions involved, from the laboratory to the clinic to data processing, have been focusing entirely on CoVac-1 in recent months.
T-cell activator triggers continuous immune stimulation
Peptides are water-soluble molecules that need to be well packaged in order to exert their full effect in the body. Walz explains: "The peptides themselves only slightly stimulate the immune system and would be degraded within about 24 hours. We therefore mix them with the adjuvant XS15, which was developed by Prof. Rammensee in cooperation with a company called EMC Microcollections GmbH. This mixture enables us to induce unusually strong immune responses." XS15 is the first water-soluble adjuvant and can be combined with any peptide cocktail. Mixing the solution with the oil montanide before application induces the formation of a granuloma, which acts like a depot from which the peptides are released over months, thus enabling long-lasting immune stimulation.