Between conservative and surgical intervention
Innovative tubular prosthesis enables reversible treatment for type 2 diabetes
Severe obesity is considered a major cause of type 2 diabetes. Building on gastric bypass surgery, the Mannheim-based company Trans-Duodenal Concepts has developed an endoscopically implantable tubular prosthesis that lines the duodenum. This both reduces food intake and can restore normal blood sugar metabolism.
Diabetes mellitus is a chronic metabolic disorder in which the insulin-mediated uptake of glucose into the body’s cells is impaired, leading to persistently elevated blood sugar levels. While type 1 diabetes results from an autoimmune reaction that destroys the insulin-producing beta cells in the pancreas, type 2 diabetes is caused by reduced sensitivity of the body’s cells to the hormone. High blood glucose levels cause sugar to irreversibly bind to plasma proteins and membrane components, which leads to long-term blood vessel and nerve damage. If left untreated, the disease can result in blindness, kidney failure, heart attack, stroke or severe circulatory disorders in the lower limbs.
According to the World Health Organization (WHO), approximately 830 million people worldwide had diabetes in 2022, more than four times as many as in 1990.1) Over 95 percent of those affected had type 2 diabetes. In 2021, more than two million deaths were directly linked to the disease or diabetes-related kidney damage.
Obesity often leads to diabetes
 Trans-Duodenal Concepts GmbH (left: CEO Prof. Dr. Georg Kähler) intends to launch the Trans-Duodenal Barrier on the market in the near future with the support of Ovesco Endoscopy AG (right: CEO Prof. Dr. Marc Schurr). © Trans-Duodenal Concepts GmbH
Trans-Duodenal Concepts GmbH (left: CEO Prof. Dr. Georg Kähler) intends to launch the Trans-Duodenal Barrier on the market in the near future with the support of Ovesco Endoscopy AG (right: CEO Prof. Dr. Marc Schurr). © Trans-Duodenal Concepts GmbHLifestyle plays a decisive role in the development of type 2 diabetes. Smoking significantly increases the risk of developing the disease, as nicotine impairs both insulin production and its effect.2) However, the primary cause is obesity - that is, being severely overweight with a body mass index (BMI) over 30. This is because years of hypercaloric nutrition overwhelms the metabolism. In addition, low-level inflammatory reactions in fatty tissue can activate the immune system, leading to the release of signalling molecules that disrupt blood sugar metabolism.3)
The latest research also shows that elevated plasma levels of the peptide hormone adrenomedullin in overweight individuals inhibit insulin receptors in the walls of the blood vessels. This reduces tissue perfusion and, consequently, the transport of insulin and nutrients to the organs.4) Weight reduction measures are therefore a central component of type 2 diabetes therapy. "Obesity is a chronic disease, not a character flaw," explains Prof. Dr. Georg Kähler of Trans-Duodenal Concepts GmbH (TDC) in Mannheim. The company that Kähler founded in 2018 has developed an innovative, easy-to-use product for treating obese diabetics based on surgical procedures.
Tubular prosthesis simulates bypass surgery
Surgical treatments for obesity not only promote significant weight loss but, in most cases, also reduce blood sugar levels more effectively than medication or dietary changes.5) In a sleeve gastrectomy, the volume of the stomach is surgically reduced, whereas in a gastric bypass, a portion of the stomach is bypassed and reconnected to the small intestine beyond the duodenum. Both procedures reduce food consumption and consequently calorie intake, while bypassing the duodenum also reduces digestion and nutrient absorption.
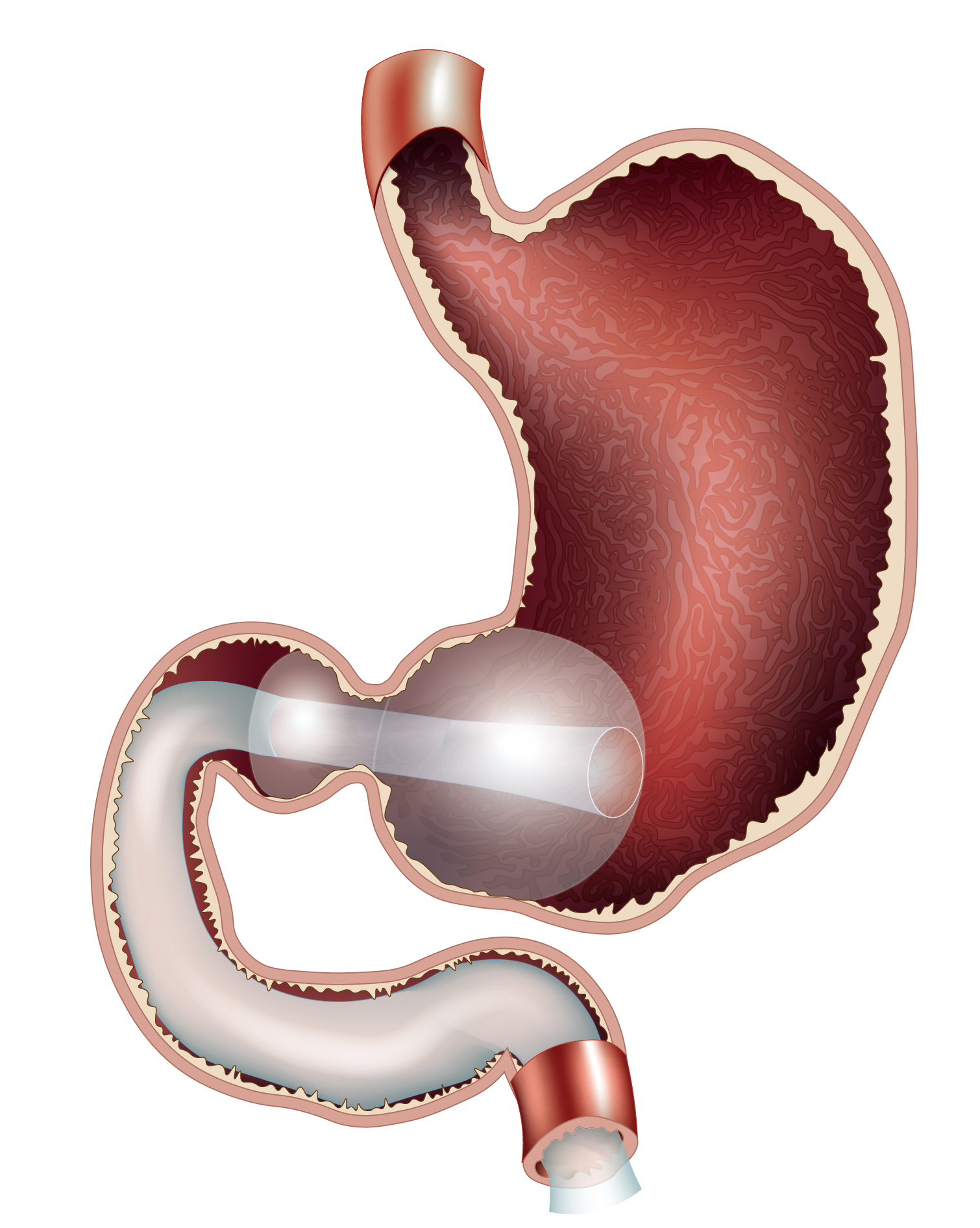 The Trans-Duodenal Barrier is an endoscopically implantable tubular prosthesis made of polyurethane that is fixed to the gastric outlet with two air-filled balloons and lines the duodenum. © Trans-Duodenal Concepts GmbH
The Trans-Duodenal Barrier is an endoscopically implantable tubular prosthesis made of polyurethane that is fixed to the gastric outlet with two air-filled balloons and lines the duodenum. © Trans-Duodenal Concepts GmbH"Interestingly, blood sugar levels improve within a few days, especially after bypass surgery, and long before significant weight loss occurs," says Kähler. "This is because the altered gastrointestinal passage affects intestinal hormone production and consequently overall metabolism. Satiety hormones such as GLP-1 are released in greater quantities, and insulin levels normalise."
Since both gastric reduction and bypass surgery are complex procedures that are difficult to reverse, TDC developed a well-tolerated temporary implant with comparable effects. Kähler, who has been head of the Central Interdisciplinary Endoscopy Unit at Mannheim University Hospital for many years, explains: "Our Trans-Duodenal Barrier is a tubular prosthesis made of polyurethane that is placed endoscopically at the gastric outlet and lines the duodenum. In a way that is similar to bypass surgery, it diverts food past the upper part of the small intestine." A few years ago, Kähler used a similar product at the hospital, but issues frequently arose due to the metal-containing anchoring. Nevertheless, the method was well received and so he designed a more compatible alternative. "We retained the basic principle but chose a PFAS-free material. We also developed an atraumatic fixation using two balloons positioned on either side of the gastric outlet. Our product both alters the intestinal passage and also reduces gastric peristalsis, thereby prolonging the feeling of satiety."
Approval trial has started
Over the past eight years, the Trans-Duodenal Barrier has been extensively tested for safety and practicality. The material must withstand gastric acid with a pH of 1.5, and the anchoring must remain secure without causing pressure. Following the successful completion of all preclinical tests and animal trials, a Germany-wide approval study involving obese diabetics has now begun. "We expect our product to result in greater weight loss than the previous system and to be better tolerated," says Kähler, who is an abdominal surgeon. "The 60 cm-long tube covers less than 20 percent of the small intestine wall, which is why deficiency symptoms should not occur, as they do after surgical procedures." In addition to metabolic changes, the subjective feeling of satiety among test subjects will be evaluated during the six-month implantation period.
Sophisticated safety concept
To enable early detection of Trans-Duodenal Barrier damage, the balloon positioned on the gastric side is filled with methylene blue. If the non-toxic dye leaks, the urine turns green. This necessitates prompt removal of the implant, as a dislodged implant could cause intestinal obstruction. The implant can easily be removed by any endoscopist. However, due to the double-walled, two-layer design of the balloons, the risk of damage is extremely low. The fluid filling further enhances visibility and enables highly precise ultrasound monitoring of the system.
The innovative tubular prosthesis bridges the gap between conservative and surgical treatments. Kähler explains: "Our procedure is safe, reversible, quick and straightforward. This means it can also be used on younger patients and people with lower BMI values. The implantation does not require anaesthesia or X-ray fluoroscopy and can be performed by registered endoscopists using our special applicator." The previous model demonstrated that the anti-diabetic effect can last up to three years after removal. If necessary, the procedure can either be repeated without causing complications or combined with medication. Furthermore, the implant can also help treat the inflammation associated with fatty liver disease, which is known as metabolic dysfunction-associated steatohepatitis (MASH).
TDC hopes to bring the product to market within two to three years. After initial financing from High-Tech Gründerfonds Bonn, a private investor from Mannheim and Venture-Capital-Fonds Rhein-Neckar the company is currently receiving support from Tübingen-based Ovesco Endoscopy AG.