Immunology – at the forefront of medical progress
Immunology is constantly changing with the emergence of new technologies and areas of application, and has branched out in many directions. Immunological approaches are central to everything – be it the development of innovative active substances and vaccinations against cancer, the search for new therapies against neurodegenerative diseases or autoimmune diseases, or combatting well-known infectious diseases or new virus epidemics.
In late 2018, James P. Allison from the U.S.A. and Tasuku Honjo from Japan were awarded the Nobel Prize in Physiology or Medicine for their “discovery of cancer therapy by inhibition of negative immune regulation”. They discovered immune checkpoint inhibitors, which are antibodies that prevent cancer cells from inhibiting the body’s immune response. This activates the body’s immune cells, enabling them to recognise and destroy cancer cells. The research by the two immunologists has led to a significant improvement in therapies for life-threatening cancer diseases such as malignant melanoma, renal cell cancer and non-small cell lung cancer. These new checkpoint inhibitors are currently being tested for their effect on metastatic cancers with an unknown primary tumour, for which no therapeutic recommendations are currently available. Checkpoint inhibitors have also proven effective in the treatment of allergies, autoimmune diseases and transplant rejection. However, they can also cause serious side effects.
Allison and Honjo are the latest in a long line of immunologists to be awarded the highest distinction in medicine, following on from pioneers over a hundred years ago, such as Emil von Behring, Robert Koch and Paul Ehrlich. Depending on how immunology is defined, between 35 and 56 of the 219 Nobel Prizes in Physiology or Medicine have been awarded for discoveries in the field of immunology. Like no other discipline, immunology has been repeatedly transformed and expanded through innovative technologies and new areas of application. Today, it is a cross-sectional science that has branched out in many directions, with findings from immunology permeating many other fields of biological and medical research.
Cancer immunotherapies
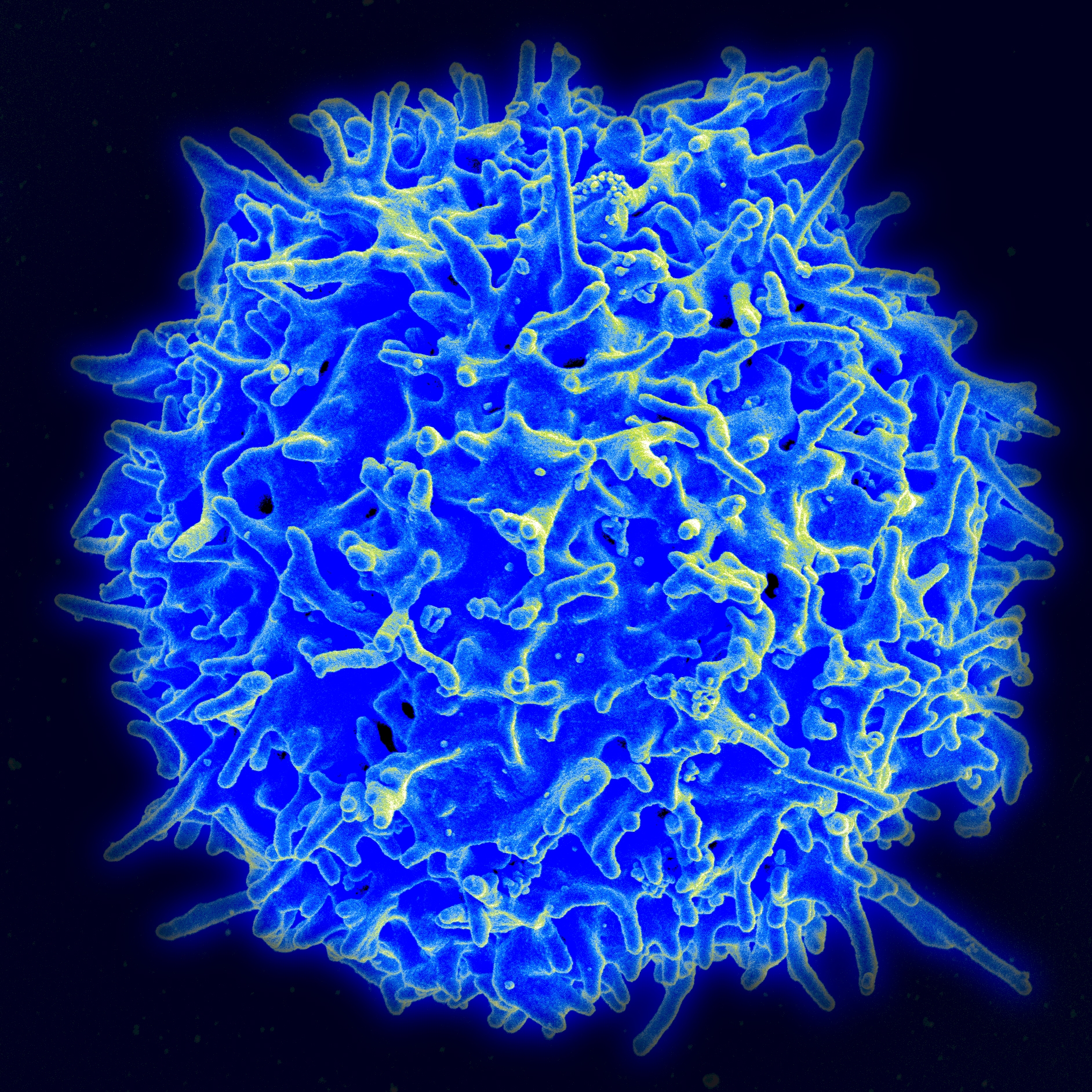 Scanning electron microscope image of a human T lymphocyte (also called T cell) from the immune system of a healthy individual. By NIAID/NIH, Public Domain, https://commons.wikimedia.org/w/index.php?curid=18233598
Scanning electron microscope image of a human T lymphocyte (also called T cell) from the immune system of a healthy individual. By NIAID/NIH, Public Domain, https://commons.wikimedia.org/w/index.php?curid=18233598In addition to the immune checkpoint inhibitors mentioned, other cancer immunotherapy strategies are being pursued. There has been initial success with bispecific antibodies, which bind to a surface molecule of T lymphocytes (thus activating them to mount an immune response against cancer), and also dock onto a tumour-specific protein (taking the immune cells directly to the site of action). This was shown for prostate cancer and non-Hodgkin's lymphoma with poor prognosis - as reported at the American Society for Hematology's annual convention in January 2020. This therapeutic approach is also an alternative to CAR-T cell therapy. It has sparked high hopes following spectacular successes in treating some highly aggressive forms of blood cancer. The therapy entails equipping an individual’s T lymphocytes with a “chimeric antigen receptor” (CAR) via gene transfer so that the cells can recognise the tumour antigens. CAR-T cell therapy is a highly complex form of treatment that can be offered by just a handful of clinics, and the successes are offset by failures that can generate serious side effects in some patients.
As Michael Baumann, Chairman and Scientific Director of the German Cancer Research Center (DKFZ), emphasises, one of the urgent tasks of cancer research is to find out why some patients react well to treatment and others do not. One way of solving this problem is through a "personalised" immunotherapy tailored to individual patients. However, this also requires personalised diagnoses. Despite commendable advances in molecular analysis technologies, it is a slow process.
The common factor with the abovementioned therapy strategies is that they rely on recruiting T lymphocytes from the adaptive immune system for the defense against cancer. There are other approaches (and initial positive experiences with metastatic colorectal cancer) that fight off cancer by activating macrophages and natural killer cells of the innate immune system.
Prophylactic and therapeutic cancer vaccinations
 One of the most important tasks in immunology is to use vaccines to prevent epidemics - Photo by Angelo Esslinger on Pixabay, Source: https://pixabay.com/de/photos/impfung-impfspritze-medizin-arzt-2722937/
One of the most important tasks in immunology is to use vaccines to prevent epidemics - Photo by Angelo Esslinger on Pixabay, Source: https://pixabay.com/de/photos/impfung-impfspritze-medizin-arzt-2722937/In 2006, a vaccine against cancer-causing human papillomaviruses (HPV) was the first prophylactic cancer vaccine to be approved by the FDA and the European Medicines Agency. It gives women almost 100 percent protection against cervical cancer if they are vaccinated before their first sexual contact. The vaccine has the potential to prevent all other tumours associated with HPV (including white skin cancer and anal cancer in men) if the vaccine is used consistently for boys and girls alike, which unfortunately is not yet the case, especially in Germany.
An estimated 50 percent of all cases of hepatocellular carcinoma worldwide are attributed to hepatitis B virus (HBV) infections, which are also responsible for acute and chronic inflammation of the liver, cirrhosis of the liver and acute liver failure. The vaccination against HBV infection, which has been available for quite some time and has been recommended in Germany for infants and children since 1995, can therefore also be regarded as a prophylactic cancer vaccine. In Taiwan, for example, where liver tumours were once very common, the incidence of this highly dangerous cancer has dropped significantly twenty years after the introduction of HBV vaccination. Hepatitis C virus infections are also associated with liver cancer. Effective therapeutic agents against this virus exist, but no vaccine is available as yet. However, intensive research is being carried out to develop an effective HBV vaccine.
A vaccine prototype has now been developed against infections with the Epstein-Barr virus, which belongs to the group of herpes viruses and is responsible for a whole range of cancers. However, it still has to be tested for use in humans. The past few years have also seen progress in the development of therapeutic vaccinations against existing infections, precancerous stages or early stages of cancer. Unlike prophylactic vaccination, this is not about the body developing antibodies against the infectious virus but instead, activating cytotoxic T cells of the cellular immune defense in such a way that they recognise and kill virus-infected and degenerate cells, but not normal body cells. Appropriate vaccines against cervical cancer and other HPV-induced cancers as well as against certain brain tumours (gliomas) have already proven effective in animal experiments.
Biotech companies in the fight against cancer
In addition to large companies such as Boehringer Ingelheim Pharma GmbH & Co. KG in Biberach near Ulm and Roche Diagnostics in Mannheim, smaller biotechnology companies with innovative technologies in the field of immunotherapy and cancer vaccination have become established in Baden-Württemberg over the past two decades. Examples are: immatics Biotechnologies GmbH, which develops bispecific T cell receptor molecules, and CureVac AG, which focuses on mRNA-based cancer immunotherapies. Both are spin-offs from the laboratory of the Tübingen immunologist Prof. Dr. Hans-Georg Rammenee. Another company is SYNIMMUNE GmbH, which focuses on novel antibodies that are effective against certain types of blood cancer. The Ochsenhausen-based laboratory Dr. Merk & Kollegen GmbH relies on the development of oncolytic viruses to fight cancer, and the Swiss-German company VAXIMM in Mannheim and Basel has developed a live oral vaccine that prevents cancer growth by inhibiting tumour angiogenesis (the blood supply to tumours).
Flu, AIDS, malaria and other epidemic diseases
 In 2018, almost half of the world's population was at risk of malaria. Most malaria cases and deaths occur in sub-Saharan Africa. - Photo by Oberholster Venita on Pixabay; Source: https://pixabay.com/de/pahotos/moskito-malaria-plakette-krankheit-1016254/
In 2018, almost half of the world's population was at risk of malaria. Most malaria cases and deaths occur in sub-Saharan Africa. - Photo by Oberholster Venita on Pixabay; Source: https://pixabay.com/de/pahotos/moskito-malaria-plakette-krankheit-1016254/Prevention of epidemics has been the most important task in immunology since Edward Jenner first vaccinated humans with cowpox serum in 1796 and Robert Koch discovered the anthrax and tuberculosis pathogens eighty years later. It is not much different today, considering the recurring threat scenarios from devastating, well-known and new epidemics.
The mutation frequency of influenza viruses and the variability of their surface antigens mean that newly adapted vaccines need to be constantly developed, and are often only available when the risk of infection is over. With broadly neutralising antibodies and virus core antigens that cause cytotoxic T cell reactions, one could perhaps achieve permanent immunity to the flu, which killed over 25,000 people in Germany in the winter of 2017/18 alone. Prophylactic vaccines against coronaviruses, which in 2019/2020 are causing global concern for the third time this century, have not yet been developed and are thus unable to prevent the primary spread of the disease.
Influenza and coronavirus pneumonias are, like Ebola, HIV/AIDS and many other infectious diseases, zoonoses that have spread from animals to humans. Research into the infection pathways and defense mechanisms in natural hosts and intermediate hosts, which are often immune to the pathogen, are an important branch of immunology. More than thirty approaches are currently being tested for treating AIDS, which was previously incurable. One can only hope that an effective vaccine will be available in the near future. New findings point to possible therapeutic targets against previously unassailable latent phases of the HI viruses in the cell nuclei of the immune cells, so that one day AIDS could actually be completely vanquished.
After tuberculosis and AIDS, malaria is the infectious disease that causes the most deaths worldwide. The hugely complicated life cycle of the malaria parasite has so far hampered the development of effective vaccines. After decades of research, there are now promising vaccine candidates. As more and more parasite strains become resistant to the best available therapeutic agents, the search for new control strategies continues. The focus is on the activation of the body's immune system. Due to global warming, there are fears that malaria and other mosquito-borne infectious diseases such as dengue and zika will continue to spread. Research into these diseases aimed at developing effective vaccines, as it is being driven forward by researchers in Heidelberg, can therefore also be seen as a preventive measure against outbreaks in Europe.
Autoimmune diseases
Another highly topical area of immunological research and development is autoimmune diseases. They are triggered by a specific adaptive immune response to the body's own antigens without the influence of a foreign antigen. These include type I diabetes, multiple sclerosis and coeliac disease, a devastating bowel disease. An autoimmune disease is nearly always a genetic predisposition; disease triggers are environmental factors such as, in the case of coeliac disease, gluten. The environmental factors for type I diabetes and multiple sclerosis are not clear; however, it is striking that the incidence of these particular illnesses has risen sharply in all advanced industrial countries in recent decades. Gut bacteria seem to play a role in the development and prevention of these diseases - via the gut immune system. One explanation for this is the “hygiene hypothesis”, originally formulated by the British doctor David Strachan for allergies. He suggested that frequent contact with bacteria and viruses in early childhood protects against allergic diseases, and such contact has become rare due to hygiene measures in highly developed industrial countries.
Immunologists from Constance have shown that a special protein complex in the cells, the immune proteasome, strengthens the immune response and can trigger an autoimmune reaction. This reaction could be suppressed by specific agents that block the immune proteasome without weakening the entire immune system, as would be the case with conventional immunosuppressants. It seems that the latest findings are coming closer to solving the fundamental question of how the body protects itself against autoimmune reactions (the “self-tolerance” of the immune system): it has been shown in mice that certain proteins (so-called annexins) released from body cells during programmed cell death (apoptosis) are recognised by dendritic cells, the most important antigen-presenting cells of the immune system. This triggers a signalling chain that ultimately suppresses an immune response.
Further dossiers on the topic
Die Aktivierung des körpereigenen Immunsystems zur Bekämpfung von Krebs ist nicht mehr nur ein vielversprechendes Therapiekonzept, sondern wird bereits in der medizinischen Praxis angewendet. Erste Immuntherapeutika sind zugelassen; viele weitere befinden sich im experimentellen Stadium oder in klinischen Studien. Impfungen zur Vorbeugung bestimmter Krebskrankheiten werden schon im großen Umfang erfolgreich eingesetzt.
Nachdem jahrzehntelang B- und T-Lymphozyten sowie Makrophagen als wichtigste Zellen des Immunsystems galten und intensiv erforscht wurden, stehen jetzt die dendritischen Zellen als Hauptkomponenten der adaptiven Immunität im Zentrum des wissenschaftlichen Interesses. Auch die Erforschung der angeborenen Immunabwehr hat an Bedeutung gewonnen, seit die Funktion der Toll-like-Rezeptoren bei dieser ersten Verteidigungslinie des Körpers gegen Fremdattacken erkannt worden ist. Die Verleihung der Medizin-Nobelpreise trägt diesen neuen Entwicklungen Rechnung.

Impfungen sind heute in Deutschland nicht besonders populär, wie sich zuletzt bei der heftig geführten Diskussion um das Für und Wider einer Schutzimpfung gegen die sogenannte Schweinegrippe (bzw. Neue Grippe) gezeigt hat. Dabei wird leicht vergessen, dass wahrscheinlich keine andere medizinische Entwicklung so vielen Menschen geholfen hat wie die Immunisierung durch Impfstoffe: von der Entdeckung der Kuhpockenvakzinierung durch Edward Jenner 1796 bis hin zu den Programmen der Global Alliance for Vaccines and Immunisation (GAVI), mit denen allein seit dem Jahr 2000 über 250 Millionen Kinder in den Entwicklungsländern geimpft worden sind und die schätzungsweise fünf Millionen Menschen das Leben retteten.